
Accurate, early cancer diagnosis matters
The James Cancer Diagnostic Center gives patients direct, expedited access to diagnostic testing and consultation with Ohio State cancer experts. Think you have cancer?
Schedule an appointment today Your source for health, wellness, innovation, research and science news from the experts at Ohio State.
Your source for health, wellness, innovation, research and science news from the experts at Ohio State.
There’s a powerful story behind every headline at Ohio State Health & Discovery. As one of the largest academic health centers and health sciences campuses in the nation, we are uniquely positioned with renowned experts covering all aspects of health, wellness, science, research and education. Ohio State Health & Discovery brings this expertise together to deliver today’s most important health news and the deeper story behind the most powerful topics that affect the health of people, animals, society and the world. Like the science and discovery news you find here? You can support more innovations fueling advances across medicine, science, health and wellness by giving today.
Subscribe. The latest from Ohio State Health & Discovery delivered right to your inbox.
Subscribe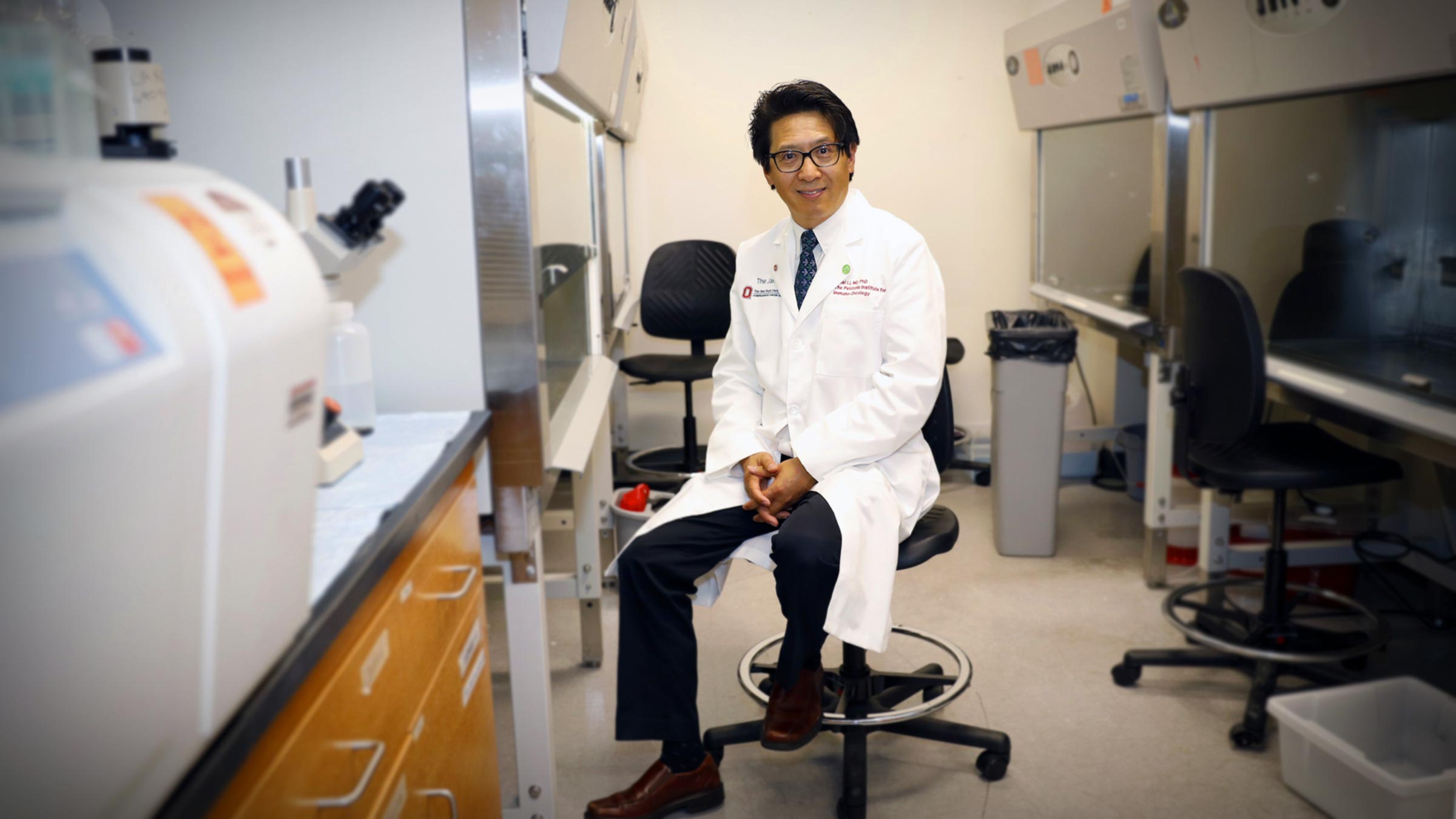
Zihai Li, MD, PhD, the founding director of the Pelotonia Institute for Immuno-Oncology at The Ohio State University Comprehensive Cancer Center – James Cancer Hospital and Solove Research Institute, is a leader in immunotherapy, which is creating transformative results for many patients who previously had few options for treating their cancer.
Cancer immunology is the study of the immune system by oncologists (cancer specialists), immunologists and other cancer researchers, and discoveries in this field help us understand that the body’s immune system can be used fight cancer. Treatments that use our own immune system as anti-cancer agents are called immunotherapies.
Immuno-oncology is the discipline of treating patients with immunotherapy, rather than through other traditional cancer treatments (surgery, radiation and chemotherapy).
Cell therapy is one type of immuno-oncology, just like drugs targeting hormone receptors are one type of chemotherapy. Broadly, cell therapy is any type of treatment that uses live cells to treat a patient’s cancer. These cells may come from the patients themselves or may be derived from another person. Scientists often modify these cells outside of the patient’s body to help them target and kill cancer cells, and then infuse them back into the patient.
By understanding the “normal” functions of the body’s immune cells, such as T cells and the aptly named “natural killer cells,” immuno-oncology involves expanding and training these cells to recognize and kill cancer cells. Then, they’re infused back into the patient as an anti-cancer therapeutic.
Many immunotherapy efforts are tied to PD-1 and PD-L1, proteins found on cancer cells that enable them to hide from the body’s immune system. We have discovered ways to turn off or block those proteins, which allow the body’s immune system to recognize and attack cancer cells.
In some cases, it can. Approximately 20% of cancer patients respond well to immunotherapy targeting “checkpoints” such as PD-1. This gives us hope, but it also means there are still a lot of things we have not yet discovered.
We want to make immunotherapy effective for treating everybody with cancer, and we also want to utilize the strategy to stop cancer from forming in the first place. This involves the creation of cancer vaccines, such as the HPV vaccine, which can block infection by HPV and prevent most cervical cancers.
At the Pelotonia Institute for Immuno-Oncology, we have a tremendous number of world-class investigators, researchers and physicians in the immuno-oncology field, which positions the The Ohio State University Comprehensive Cancer Center – Arthur G. James Cancer Hospital and Richard J. Solove Research Institute (OSUCCC – James) at the forefront of discovery.
We have labs developing cell therapeutics using T cells and natural killer cells, and we are leading a number of national clinical trials. Marcos de Lima, MD, is leading an effort to use triple CAR T cells to target three markers on cancer cells simultaneously to treat lymphoma and leukemia.
In my lab, we study GARP (glycoprotein-A repetitions predominant), a molecule similar to PD-L1 that hides cancer cells from the immune system. Research and preclinical studies have shown that we can block GARP to make tumors visible to the immune system. We don’t yet know how many cancer patients will be eligible for anti-GARP therapy, but it could be a sizable percentage of those patients who do not respond to treatment that targets PD-1/PD-L1.
My colleague Yiping Yang, MD, PhD, is also investigating the “hedgehog molecule.” Originally discovered in flies, mutations in this gene result in tiny projections resembling the spikes on a hedgehog. This mutation disrupts the signaling ability of the body’s immune system, allowing cancer cells to avoid detection. Yang’s lab is working on a clinical trial that will combine a hedgehog inhibitor with a PD-1 blocker, a multipronged strategy that could be applied to several different types of cancer including liver and lung cancer.

The James Cancer Diagnostic Center gives patients direct, expedited access to diagnostic testing and consultation with Ohio State cancer experts. Think you have cancer?
Schedule an appointment today