Microsurgery techniques advance breast cancer reconstruction and lymphedema outcomes
Complex microsurgery improves breast reconstruction and prevents a common complication of lymph node removal for patients with cancer.
An Ohio State reconstructive oncologist has devoted his career to improving quality of life for patients with cancer by developing innovative methods of restoring bodies and of easing the pain and debilitation of lymphedema.
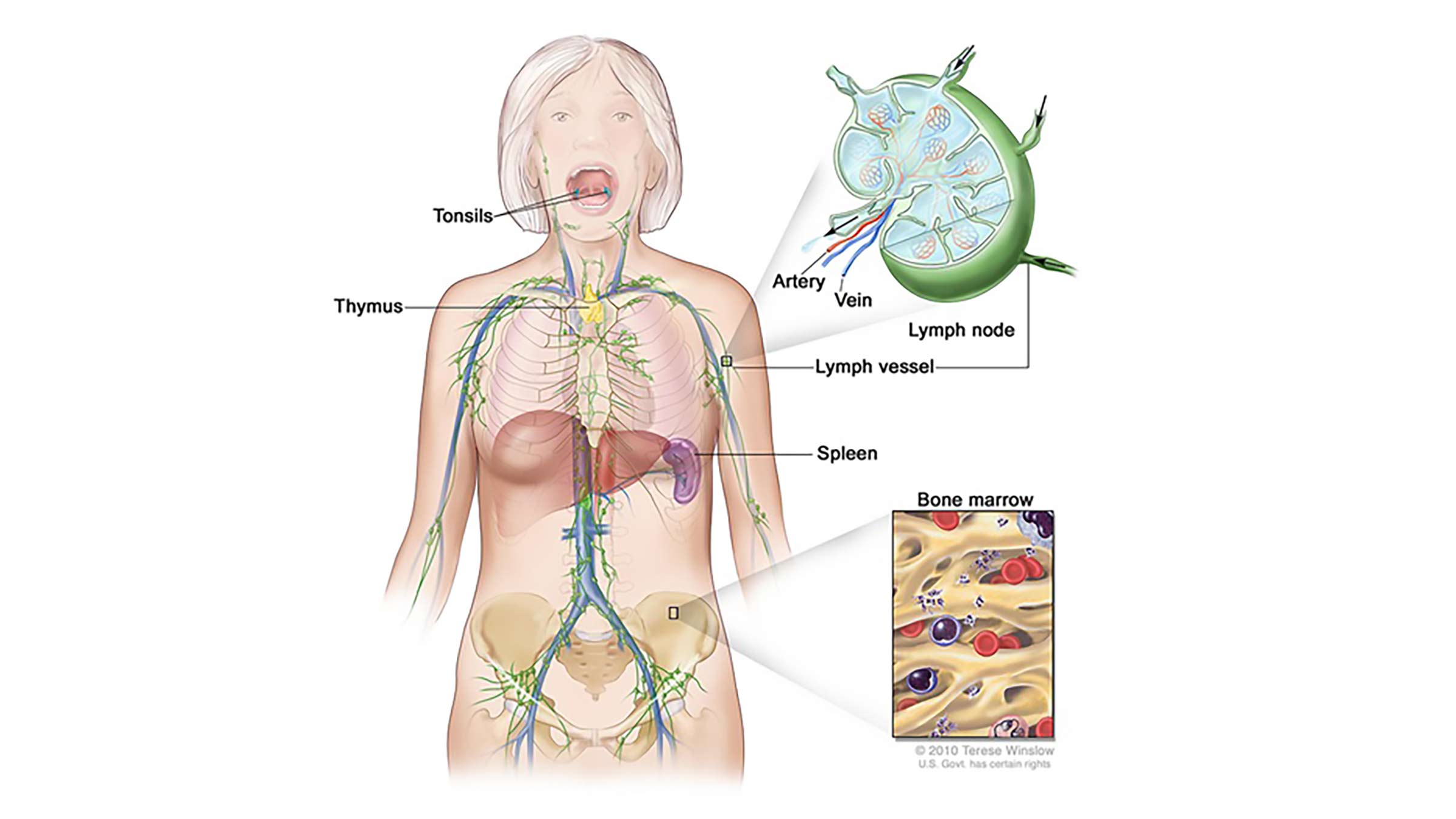
Removal of lymph nodes during cancer surgery can help determine whether the cancer has spread through the body’s lymphatic system, but the procedure also can leave patients with the painful condition called lymphedema, a chronic and debilitating swelling of the arms, legs, hands, feet or head and neck.
Roman Skoracki, MD, world-renowned oncologic plastic surgeon at The Ohio State University Comprehensive Cancer Center – Arthur G. James Cancer Hospital and Richard J. Solove Research Institute (OSUCCC – James) and his colleagues are using microsurgical techniques — some of which they developed — to treat or even prevent lymphedema.
They’re also using microsurgery expertise to improve breast reconstruction following cancer surgery by expanding their approach to selecting the right body tissue for the reconstruction.
“It’s twofold,” says Dr. Skoracki, who leads the Division of Oncologic Plastic Surgery at Ohio State and directs the Stefanie Spielman Comprehensive Breast Center at the OSUCCC – James. “We hear from our patients about their fears, desires and expectations, and I always want to exceed those, but in this team environment I constantly learn from and am challenged to improve by my colleagues.”
Dr. Skoracki adds, “It’s like a family, where you have a real sense of responsibility to everyone and never want to let anybody down. We’re very lucky to have an incredibly skilled, large team of microsurgeons who can expertly perform these procedures. We continuously learn from each other, and that helps us advance our care.”
Surgically enhancing quality of life for patients with lymphedema
An estimated 40% or more of patients who undergo lymph node removal for cancer treatment will develop secondary lymphedema, but two specialized microvascular surgeries performed by Dr. Skoracki and his colleagues, and at only a few other institutions around the country, are helping patients control or even prevent this condition.
The two surgeries are lymphatic venous anastomosis (LVA), or lymphatic bypass, and vascularized lymph node transfer (VLNT). Both involve rechanneling or reconfiguring parts of the lymphatic system to restore its impaired function, but they are distinctly different.
Lymph nodes are rounded structures that vary in size from a pinhead to an olive and are found at intervals within the lymphatic system, which returns fluid and protein molecules from body tissue to the circulatory system and plays an important role in the body’s immune defenses. Lymph nodes are clustered in the armpits, neck, genital areas and along the great blood vessels of the abdomen, among other areas.
“Cancer surgery often involves the removal of lymph nodes that are used to help determine whether the cancer has spread through lymphatic channels,” Dr. Skoracki says, explaining that such removal can impair fluid drainage from the affected area, resulting in a build-up of fluid that characterizes lymphedema.
But the LVA and VLNT microsurgeries offered at the OSUCCC – James are proving very effective at either preventing lymphedema or treating patients who develop this disorder.
“Microsurgery basically uses different parts of the body to reconstruct something that’s missing,” says Dr. Skoracki, whose microsurgical subspecialties are breast cancer, sarcomas and head and neck cancer. “We really are transplant surgeons moving blocks of tissue that contain very small blood vessels — generally on the order of 1 to 2 millimeters in diameter — into another area. We’re kind of stealing from Peter to pay Paul, using parts of the body to reconstruct an area that needs replacement.”
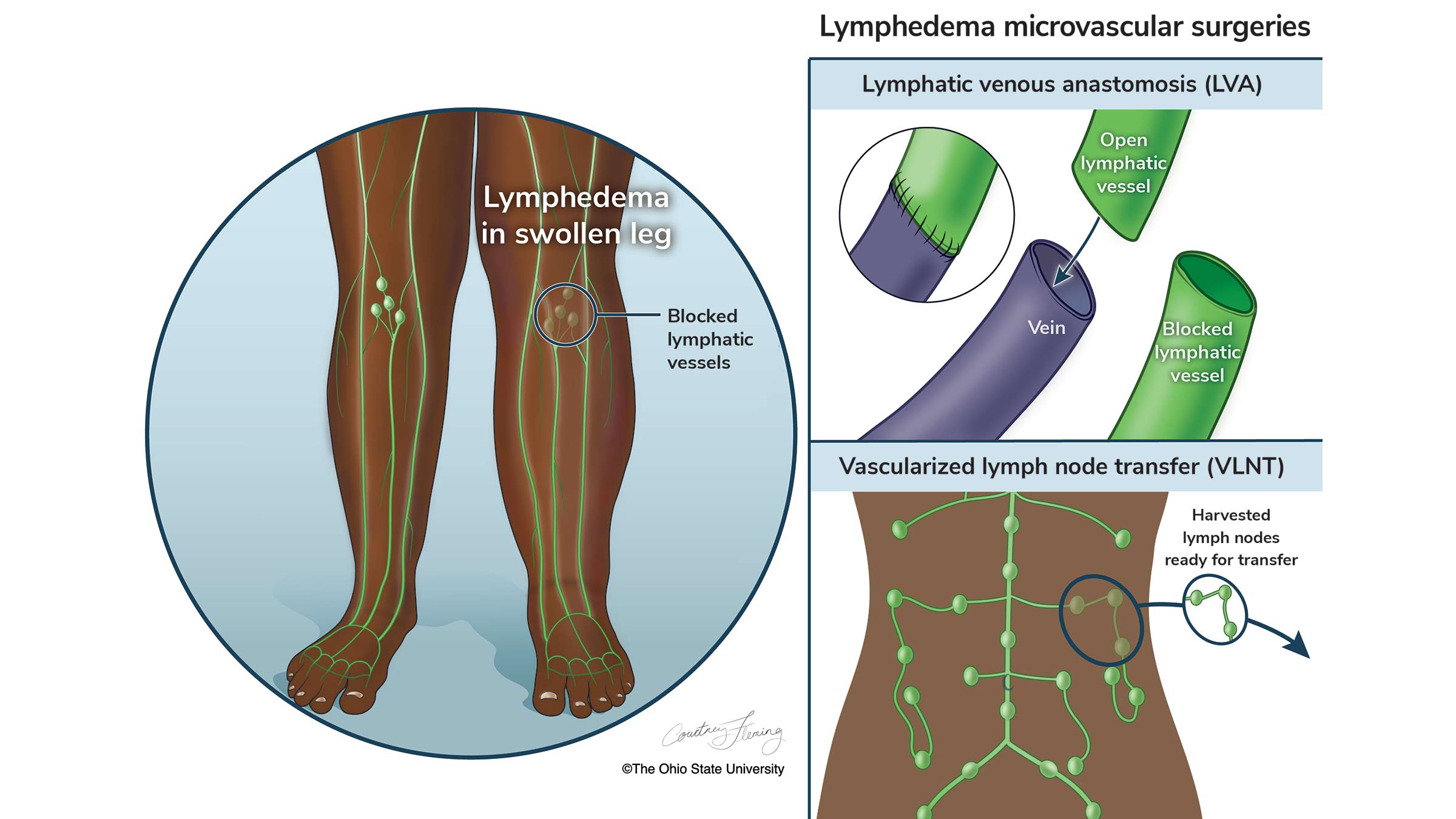
LVA, he says, attempts to recreate connections that naturally exist between the lymphatic system and the bloodstream in areas where they have been damaged by lymph node removal. “We utilize a super-microsurgical technique to create tiny shunts between lymphatic channels and blood vessels that carry fluid around the blocked areas. The rerouted fluid is then dumped into the bloodstream, which has the capacity to take on a significantly greater amount of fluid than it usually carries.”
Dr. Skoracki took part in a 2013 study published in the journal Plastic and Reconstructive Surgery that involved 100 patients who underwent the then-new LVA. The study found improvement in 96% of patients and was especially effective for those with early-stage lymphedema in their arms and hands.
“We now offer this approach preventively to high-risk cancer patients to minimize their risk of developing lymphedema. By performing this procedure at the time of a lumpectomy or mastectomy, in cases of breast cancer, we can lower a patient’s risk of developing lymphedema by five- to tenfold,” Dr. Skoracki says.
He notes that OSUCCC – James microsurgeons were among leaders in adopting this immediate lymphatic bypass to help prevent lymphedema and are still among only a few specialists in the country who have extensive experience with it. “But because our results are so promising and we’re sharing them, thankfully this procedure is being adopted more widely.”
LVA is not an option for patients who have no functioning lymphatic channels to connect to in the affected region. Dr. Skoracki says these patients may be candidates for the even newer VLNT procedure, which reintroduces lymph nodes into an area where they have been removed.

“We transplant lymph nodes from an unaffected area of the body and attach them to a blood supply in the affected area,” he says. “Then the lymph nodes themselves sprout connections and release a growth factor that attracts the growth of lymphatic channels toward them as well. So, this procedure essentially recreates a functioning lymphatic system by replacing what’s been lost.”
In one approach to VLNT, Dr. Skoracki says, OSUCCC – James microsurgeons are true pioneers: They were the first team to harvest and transplant lymph nodes from the body’s mesentery, a fan-shaped tissue in the abdomen, and were among the first to use the omentum, an apron-shaped tissue rich in lymphatics, also in the abdomen.
“The mesentery has a great number of lymph nodes embedded in it, and we can harvest small clusters of nodes from it without causing lymphedema at the site from which we take them,” he says, adding that this approach also has caught on at medical institutions globally. “Both of these have been widely adopted by many centers around the world as a go-to for lymphatic reconstruction.”
Overall, he says, these procedures are gaining more and more traction among medical institutions, but not always “to the full breadth that is available here. There are probably between five and 10 centers around the country that offer patients the entire breadth of microsurgical intervention that we offer.”

Refinement through research
The OSUCCC – James has a team of seven microsurgeons who can perform these intricate procedures, which they continuously refine and improve via research.
“We’ve looked at several research projects related to lymphedema,” he says. “For example, we’re looking at our experience with performing immediate lymphatic reconstruction at the time of axillary node dissection (the removal of lymph nodes from the armpit, or axilla).
“In the past two years, we’ve examined over 150 patient outcomes to confirm that this procedure has a significantly positive impact on quality of life,” Dr. Skoracki says.
Dr. Skoracki’s research specialties include clinical outcomes of breast, sarcoma and head and neck cancers. His team is excited to have recently submitted a U.S. Department of Defense grant proposal for funding to study head and neck lymphedema.
“Patients with head and neck lymphedema are really an underserved population,” Dr. Skoracki says. “There are only a very few centers in the world that have looked at this and are working on it, and we’re certainly among those.”
Advancing breast cancer reconstruction
OSUCCC – James research has opened avenues of innovation in breast reconstruction as well.
“It’s exciting that we’ve really expanded our palette of offerings to patients needing breast reconstruction after surgical treatment, specifically in what we call autologous reconstruction.”
“Traditionally,” Dr. Skoracki explains, “we offered the lower abdomen as a donor site to recreate a breast for patients wanting to use their own tissue for this procedure. Now, we’re using multiple donor sites around the body to reconstruct a breast to give the best aesthetic outcome and the best match to both the preoperative breast and the other breast, depending on whether it’s a unilateral (single breast) or bilateral (both breasts) reconstruction.”
He says surgeons can now remove tissue from thighs, the lower back and other body sites to try to minimize donor-site disruption and optimize quality of life for patients. “There are not many places in the country that offer such innovative approaches to breast reconstruction,” he adds.
Advancing the vision
Nearly a decade has passed since Dr. Skoracki was recruited to the OSUCCC – James from MD Anderson Cancer Center in Houston, a move that he considered “a tremendous opportunity” for him and his family.
“I love the vision of the OSUCCC – James,” he says. “I love the highly individualized care we give to each patient, not just at the level of providing surgery or medications, but also as a unique person.
“And, as I’ve said, the family atmosphere at our institution drives you to succeed … you never want to disappoint anyone.”
With his innovative surgical skills and compassion for all, he likely never will.

Accurate, early cancer diagnosis matters
The James Cancer Diagnostic Center gives patients direct, expedited access to diagnostic testing and consultation with Ohio State cancer experts.
Schedule an appointment today



