Advanced robotic surgery giving pancreatic cancer patients 'the gift of time'
Mary Dillhoff, MD, is part of an elite group of surgeons leveraging robotic technology to improve outcomes for patients with some of the deadliest forms of pancreatic, liver and bile duct cancers.
In 2019, Zosay Washington was admitted to the emergency department at The Ohio State University Wexner Medical Center with a case of severe itching all over his body.
A former American Airlines worker and gospel recording artist, Washington was in his late 60s and enjoying retirement. He and his wife were preparing to embark on a Caribbean cruise, so he hoped that nothing was seriously wrong.
Doctors performed a series of tests. When the results came back, Washington’s world was blown apart. The diagnosis: pancreatic cancer. In cases where a pancreatic tumor blocks the body’s bile duct, bile backs up in the liver and leads to the severe itching he was experiencing.
He was quickly referred to Mary Dillhoff, MD, a surgical oncologist at The Ohio State University Comprehensive Cancer Center – Arthur G. James Cancer Hospital and Richard J. Solove Research Institute (OSUCCC – James) and associate professor of Surgery at The Ohio State University College of Medicine. An early leader in performing robotic procedures to treat pancreatic cancer, Dr. Dillhoff was one of only a few surgeons with the experience and expertise to treat Washington through robotic-assisted surgery.
“I was nervous heading into surgery, but I had no hesitation after talking with Dr. Dillhoff,” Washington says. “She was so congenial; she walked me through the whole thing and told me exactly what was going to happen. And when the CT scan shows that you have cancer, what else can you do?”

Building expertise in hepato-pancreato-biliary (HPB) surgery
Dr. Dillhoff specializes in performing complex procedures for cancers of the pancreas, liver, bile duct and stomach.
“I dreamed of going into medicine as a kid, but it was uncommon for women in my area to go to college, let alone medical school,” she says of her upbringing in rural northwest Ohio. Fortunately, a local family doctor took her under his wing and let her shadow him at the hospital during her high school years. Inspired by his service to her community, she resolved to follow in his footsteps and return home to practice family medicine after attending medical school.
At the University of Cincinnati College of Medicine, her plans changed when she began her surgery rotation. “I thought it was going to be difficult and just wanted to get it done,” she remembers. It was difficult, but she loved every moment of it. There was something immensely satisfying about performing a technical feat with an immediate outcome. After medical school, she entered residency in general surgery at The Ohio State University Wexner Medical Center.
During her residency, she spent two years in the laboratory of Mark Bloomston, MD, a former surgical oncologist at the OSUCCC – James. The prospect of finding surgical and therapeutic solutions for patients with some of the most devastating forms of cancer was so appealing that she decided to pursue a fellowship in surgical oncology at Memorial Sloan Kettering Cancer Center in New York.
In the early 2010s, her field was gradually shifting toward using more minimally invasive techniques, including laparoscopy and robotic surgery. Robotic surgery was still in its infancy, but she had the opportunity to learn the basics through gynecological surgery.
When she returned to Ohio State in 2014 to practice surgical oncology, she spotted an opportunity to use some of the techniques she had learned during her fellowship. “Ohio State was an early pioneer in minimally invasive surgery, so there was plenty to build upon,” she says.
Dr. Dillhoff found it challenging but achievable to use robotic techniques to perform a distal pancreatectomy, a surgery to remove a tumor from the body or tail of the pancreas, as well as liver resections to remove liver tumors.
The robotic Whipple — an advanced procedure used to treat pancreatic cancer — was another story.
Inside the robotic Whipple
Every year in the United States, more than 60,000 people are diagnosed with pancreatic cancer. The disease is famously challenging to detect and diagnose early, largely because most patients experience symptoms only when the pancreatic tumor has grown to a considerable size or the cancer has spread to other organs. The symptoms they do experience, including abdominal and back pain, weight loss, jaundice, nausea and recent-onset diabetes, can be disguised within a variety of conditions.
For the minority of patients who qualify for surgery for pancreatic cancer, the pancreaticoduodenectomy — commonly referred to as the Whipple procedure (named after its surgical pioneer, Dr. Allen Whipple) — offers the best possible chance at a full recovery. The Whipple procedure involves removing the head of the pancreas, the first part of the small intestine, a portion of the bile duct and the gallbladder before reconstructing each organ. It is the single most effective treatment for pancreatic cancer and precancerous lesions, but it is also one of the most daunting procedures for any surgeon to perform.
Back in 2014, few surgeons had attempted a robotic version of the procedure. But when Timothy Pawlik, MD, PhD, MPH, chair of the Department of Surgery, expressed his intention to create a robotic Whipple program at Ohio State, Dr. Dillhoff got to work.
She and a former Ohio State colleague, Carl Schmidt, MD, returned to “Surgery 101” by observing surgeons at other medical institutions and using simulators and fake biotissues to practice the procedure. “By practicing so much beforehand, we were able to shift our learning curve,” Dr. Dillhoff says. “Our goal was to create a program that was both safe and sustainable for our patients.”
In 2017, a team led by Dr. Dillhoff and Dr. Schmidt made headlines by performing the first robotic-assisted Whipple procedure at Ohio State and one of the first in the region.

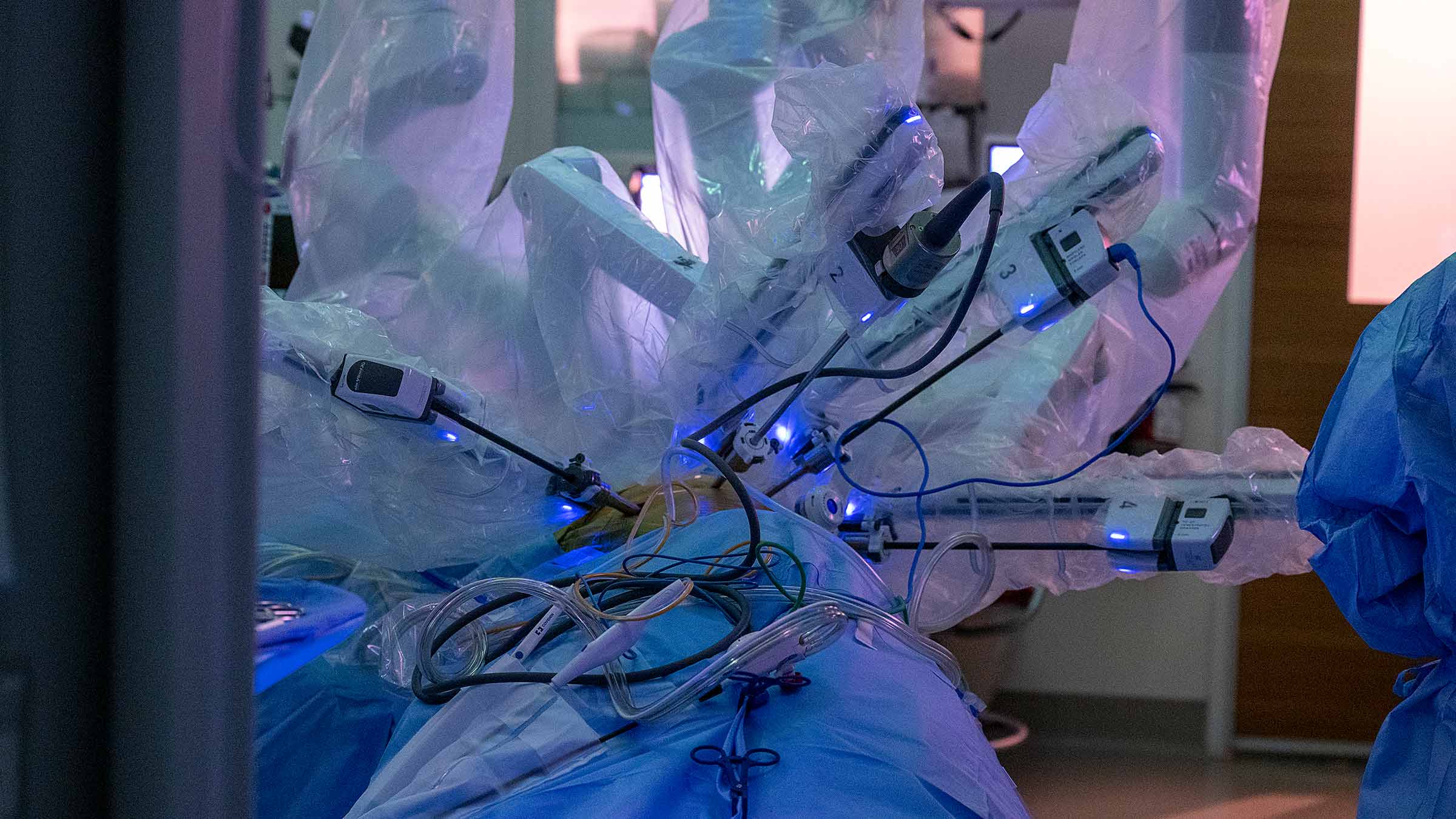
Most Whipple procedures in the United States are still open procedures, which involve making a 10- to 12-inch incision that runs from the breastbone to below the belly button. By using a four-armed da Vinci robot, Dr. Dillhoff and her team can reduce the risk of infection and scarring by making five to six incisions of approximately one-third of an inch in length instead of one larger incision.
Robotic-assisted surgery keeps the surgeon in complete control of the procedure. Sitting at a console a few feet from the operating table, Dr. Dillhoff controls the four arms of the robot. One arm is outfitted with a tiny 3D camera, which enters the abdominal cavity and provides detailed views of ducts as small as 1 millimeter in diameter. The other three arms are outfitted with instruments that let her cut, sew and move organs around to reach the pancreas.
The robot’s arms are ambidextrous and can rotate 270 degrees, affording a significantly greater range of motion than a human wrist.
Under the control of an experienced surgeon, the robot’s nimble, precise movements produce better results than any human could achieve. While robotic-assisted surgery is not the best option for everyone, patients typically experience reduced blood loss and faster recovery times after a robotic procedure. They can return to normal life a week or so earlier with fewer long-term complications and risks.
In only a few years, Ohio State has emerged as a national leader in performing the robotic-assisted Whipple procedure and other robotic HPB surgeries. Now, five out of the six members of the surgery group routinely use robotics for half of their pancreas operations.
“Dr. Dillhoff is the cornerstone of our program,” says oncologist Ashish Manne, MBBS, an assistant professor of Internal Medicine who works closely with her. “It might sound cliché, but she is great at her job. We never have to second-guess her opinion or expertise."
Next frontiers in pancreatic cancer treatment
Pancreatic cancer remains the third deadliest form of cancer in the United States. Most patients do not qualify for surgery, because they usually receive a diagnosis after the cancer has already spread. Of the patients who do undergo a combination of surgery and chemotherapy, 30-40% are alive at the five-year mark.
“Caring for patients is my greatest joy. Without a doubt, the toughest part of the job is when we can’t treat a tumor with surgery. It is an emotionally devastating situation,” Dr. Dillhoff says.
Outside the operating room, Dr. Dillhoff is dedicated to improving the survival rate for pancreatic cancer in two primary ways: enhancing patient care and translational research.
She’s co-director of the Pancreatic Cancer Multidisciplinary Clinic, where patients with pancreatic cancer receive comprehensive, research-based care in one place. In one day, they undergo diagnostic testing, blood tests and individual assessments with a team of oncologists, radiologists and social workers. “This clinic allows patients to receive a treatment plan in a very short amount of time,” Dr. Dillhoff says. “By getting all of our services aligned, we can improve outcomes for patients by getting them into surgery or chemotherapy even faster.”

From Dr. Dillhoff’s perspective, the next leap forward in her field will come from understanding the gene mutations in patients with pancreatic cancer and developing better therapeutic drugs to treat them. Pancreatic cancer is much more drug-resistant than most types of cancers, and drug development lags behind surgical advancement.
“Ultimately, more patients will be able to get surgery if our drugs work better,” Dr. Dillhoff says. “There is so much room for discovery and improvement.”
In the meantime, she will continue to change her patients’ lives in the operating room.
After undergoing a successful robotic Whipple surgery in 2019, Zosay Washington underwent six months of chemotherapy to treat his pancreatic cancer. Against the odds, the cancer has never returned. “I give the credit to God but tell the world about Dr. Dillhoff, because there are not a lot of doctors who do what she does,” he says.
“Our goal is to give every patient the gift of time. They get to attend the weddings of their children and meet their grandchildren. They live longer and better. That’s what keeps us moving forward,” Dr. Dillhoff says.

Accurate, early cancer diagnosis matters
The James Cancer Diagnostic Center gives patients direct, expedited access to diagnostic testing and consultation with Ohio State cancer experts.
Schedule an appointment today





