
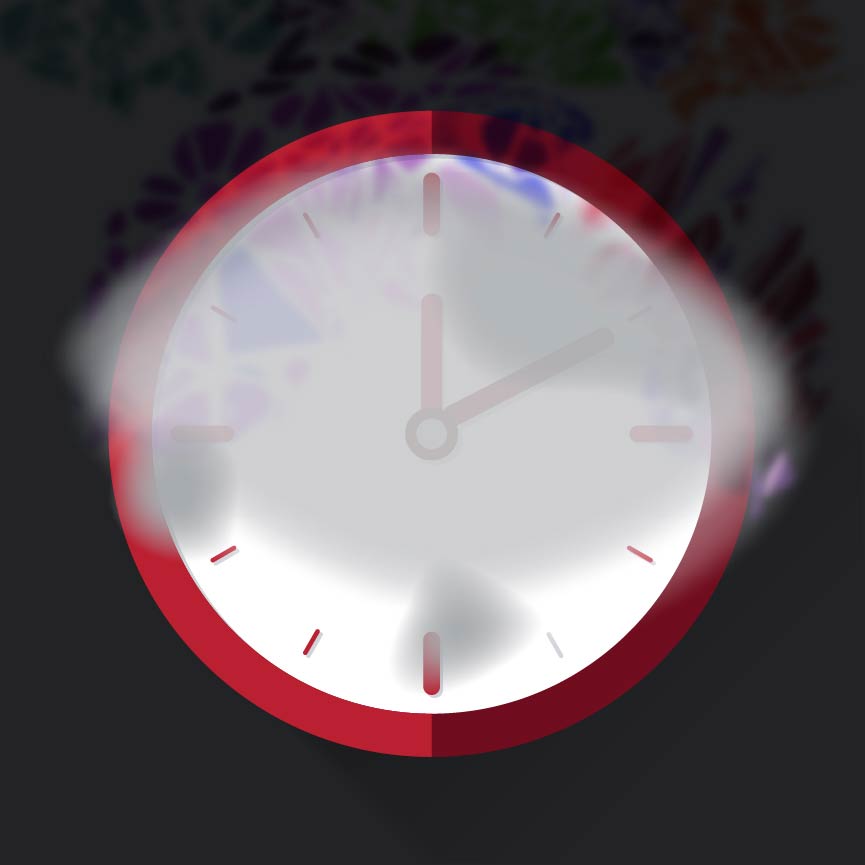
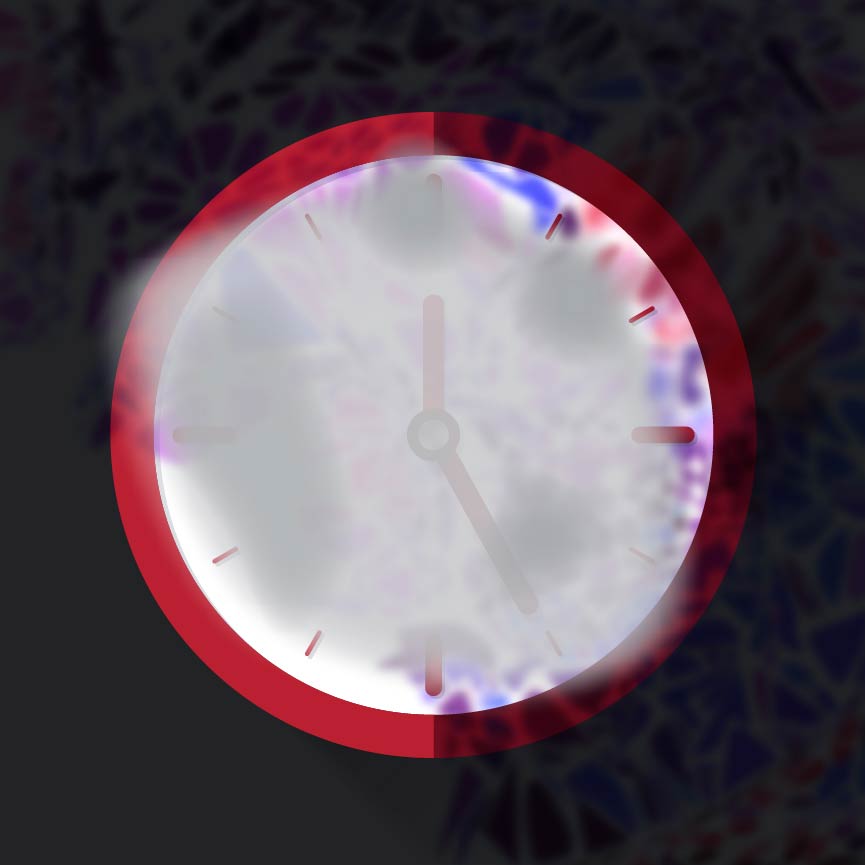
The first time you experience an ocular migraine or a migraine with aura, it can be jarring. Some people might wonder if what they’re feeling and seeing is a stroke or retinal detachment.
The good news is that, while they can be a scary experience at first, these migraines don’t seem to cause damage to the eye.
What is an ocular migraine?
An ocular migraine is what we call certain visual disturbances that can occur with or without a headache. “Migraine with aura” often refers to a headache accompanied by a wave of brain activity that most often causes visual disturbances, but can also cause auditory or olfactory (smell-based) symptoms. In a migraine with aura, the headache usually shows up after you experience visual symptoms.
These vision changes can look like flashes of light, zigzag patterns, rainbow or shimmering spots or stars, or even blind spots. They can look like zigzag rings or half-circles of flashing rainbow colors that change size.
What’s happening in the eyes or brain during an ocular migraine?
The pathway physiology or reason you get a migraine in the first place can be complex, and triggers can include any number of environmental or hormonal factors, such as allergies, certain foods, lack of sleep, dehydration, alcohol, smoking, oral contraceptives, etc. The visual migraine could be caused by spasms in blood vessels — constricting and re-dilating — or because of certain chemical changes in the brain, coming in waves.
Is it a stroke, migraine or retinal detachment?
Typically, there are a few things to look for that tell me a patient has experienced an ocular migraine or a migraine with aura.
Visual disturbances with migraine usually last between five minutes and an hour, with 20-30 minutes being what I hear most often from patients. Migraine with aura will often have a headache come afterward.
If there’s slurred speech, muscle weakness or other neurological signs along with the vision changes, that could signal something more serious, such as a stroke.
Retinal detachment is another serious condition that can have some similar symptoms to ocular migraine or migraine with aura. In retinal detachment, a layer of tissue at the back of the eye (the retina) pulls away from the other tissues in its normal position.
Classic signs of retinal detachment are flashes of light and “floaters.” Flashes can come and go, but typically floaters remain. People experiencing retinal detachment might see color changes or black curtains over their vision, and these symptoms usually last much longer than the 30 minutes most typical with migraines.
We can’t rule out the possibility of retinal detachment without a dilated eye exam, especially if you’ve never had a migraine with visual symptoms before. And although retinal detachments are rare, they can cause blindness, so it’s important to see your primary care provider or an eye doctor after experiencing these symptoms so that treatment can begin quickly if needed.


What to do if you think you’re experiencing an ocular migraine or migraine with aura
Look for whether your visual symptoms are mostly blind spots or flashes of light, or if you’re seeing floaters that aren’t going away. Take note of what you were doing before the symptoms started, in case you’ve encountered a migraine trigger.
Take note also of whether visual changes are happening in just one eye or in both eyes and at what time the symptoms began. Details of symptoms can be helpful to tell your doctor later so that you can work together on a treatment plan or in preventing future migraines.
These episodes can be visually debilitating, and some people simply can’t function either during the visual symptoms or during the accompanying headache. You might need help from loved ones in your household or from nearby co-workers if you can’t see or fully function for a time.
What to do after a migraine with visual symptoms
Once my patients have more than one migraine like this, they’re typically able to recognize the symptoms and don’t need to be examined each time, unless the symptoms change. But if you’re experiencing this for the first time, it’s best to see a doctor.
It’s best to first see an eye doctor — many primary care providers will send patients to an eye doctor for a dilated eye exam to rule out retinal detachment. Eye doctors like me often co-manage patients’ care plans with their primary care providers, who usually prescribe the medications to treat migraine. If migraines are particularly severe or frequent or have unusual symptoms, you might see a neurologist, but that typically requires a referral from another doctor first.
It may also be helpful to talk with your family members about migraines, because migraines and their symptoms are often hereditary. Other members of your family might understand what you’re going through, or your symptoms can help them know what to look out for in themselves — migraines often start around the onset of puberty or shortly after and peak in your 30s.

Great vision starts here
Ohio State's optometry clinics provide world-class eye care for your entire family.
Schedule an appointment




