What the pandemic changed — for good
Ohio State health experts reflect with optimism on how COVID-19 shaped the future
Despite the destruction of the deadly COVID-19 virus, a global pandemic led to some long-term, positive changes for health and health care.
Society was forced to adapt to a new reality and, in some ways, these adaptations will benefit us all for many years, long after the threat of COVID-19 has faded.
Hear perspectives from experts across The Ohio State University as they detail some of these “silver linings” of the past two years:
The scientific community aligned and mobilized in new ways
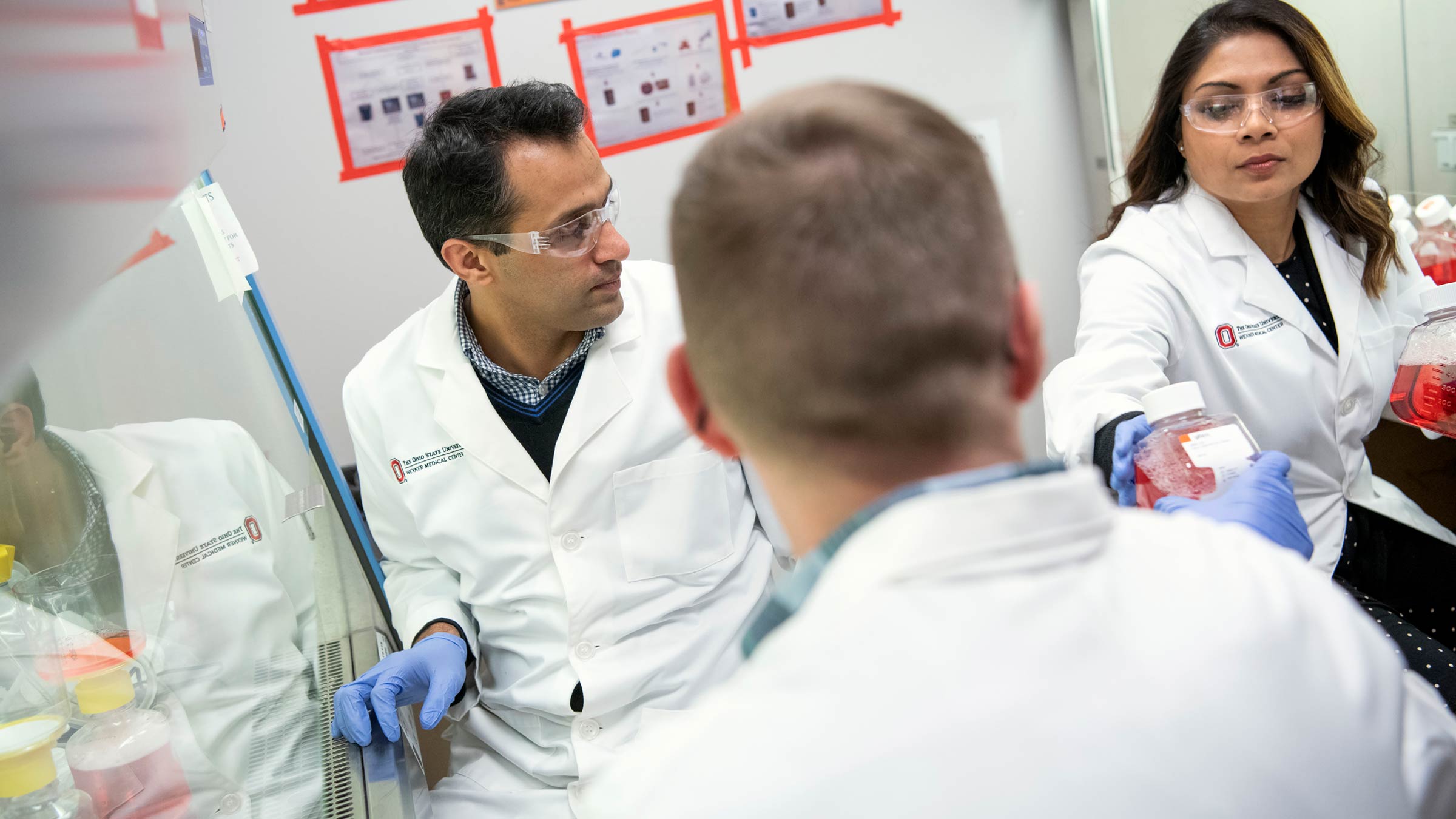
“In the COVID-19 pandemic, we’ve experienced a paradigm shift as scientists, really reasserting our critical role in the world.
“Across the world, instead of competing with other research institutions, more of us began to ask ourselves how we could work together. I feel that scientists were less concerned about their names being on published papers and more concerned with creating impact. I hope that’s something that’s not going to go away.
“In part due to the pandemic, scientists began to think of solutions more globally — not as a state issue, not what our flag or mascot is — and began thinking more with a sense of urgency.
“We learned some lessons about how quickly we could speed processes like testing and vaccine development if we removed certain barriers, reused existing technologies and worked to complete some processes simultaneously when previously we might have taken turns. It’s like having a Thanksgiving dinner with 16 people cooking and setting the table and doing dishes instead of one person doing it all. It’s not that the dinner is any worse or better, but it's done more efficiently.
"At Ohio State during the pandemic, it was never about ‘us versus them.’ It was about ‘we’ — how are ‘we’ going to fix this or solve that? The teamwork was inspiring.
“All throughout the COVID-19 pandemic, there have still been people impacted by cardiovascular disease and cancer, for example. As we emerge from the pandemic, it's important that we apply these same concepts to work together to tackle the diseases that continue to claim lives. We see now how much more we can harness from our scientific community to solve these issues.”
— Peter Mohler, PhD, vice president for Research, the John H. and Mildred C. Lumley Chair in Medicine at The Ohio State University and chief scientific officer at the Ohio State Wexner Medical Center.
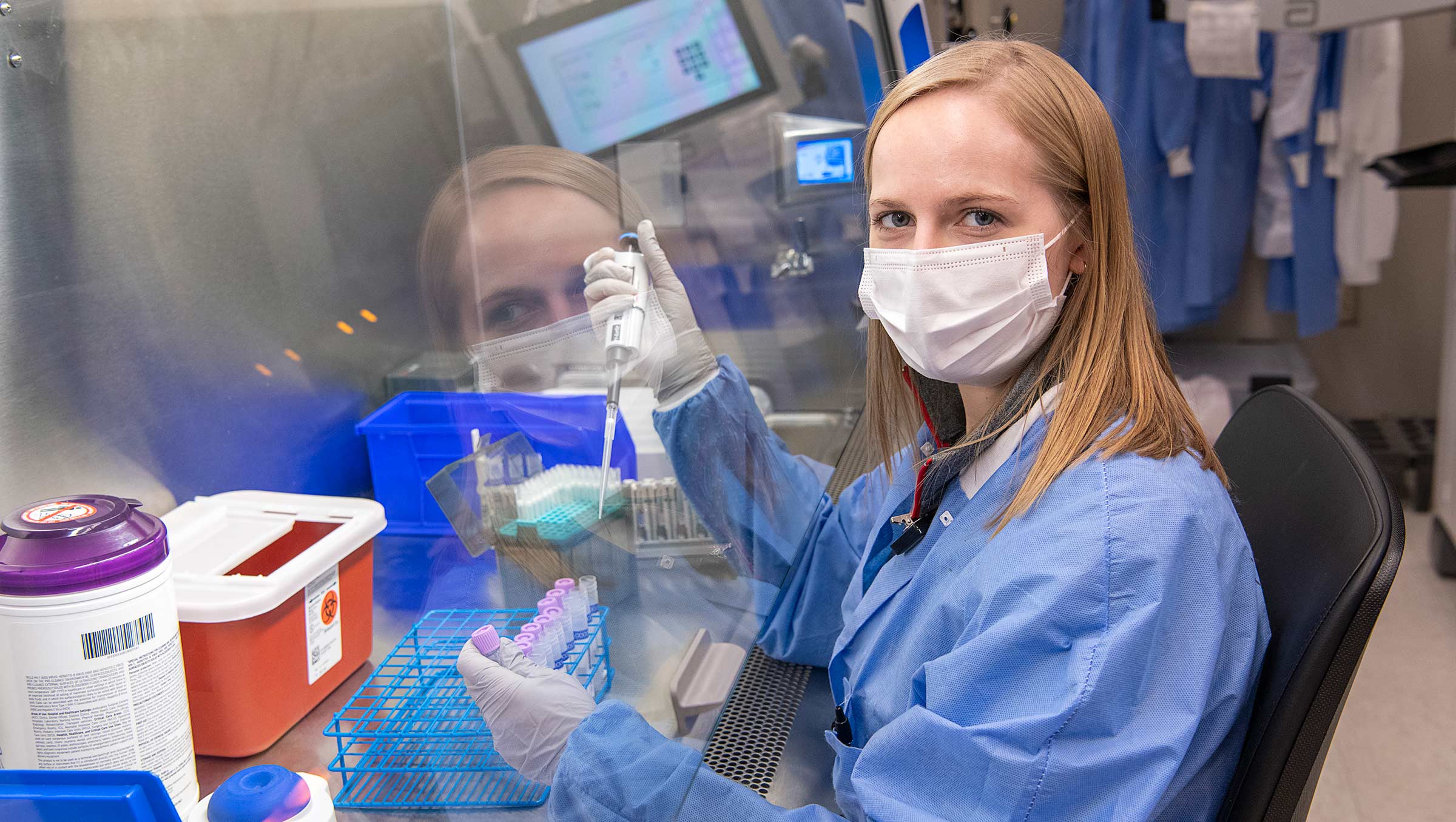
“The research community all over the world rapidly pulled together to tackle COVID-19 with an unprecedented degree of collaboration and cooperation. Here at Ohio State, for example, we saw a need for a multidisciplinary team of investigators to study the impact of COVID-19 on first responders, frontline health care workers and their household contacts. In the course of a month, we marshaled personnel and resources from all over the university and submitted a $10 million proposal to the National Institutes of Health.
“Our proposal was quickly funded, and The Ohio State University Center to STOP-COVID has been working nonstop making discoveries that increase our knowledge of how the virus behaves and disrupts people’s lives. The pandemic forced us to develop new, more efficient ways of communicating, collaborating and conducting research. We assembled our team virtually and continue to conduct our high-level work this way as much as possible. It showed us that we can be much more nimble and creative in how we operate, and this will continue to improve our productivity in the future.”
— Eugene Oltz, PhD, chair of the Department of Microbial Infection and Immunity, Samuel Saslaw Professor of Infectious Diseases and principal investigator in The Ohio State University Center for Serological Testing to Improve Outcomes from Pandemic COVID-19 (STOP-COVID)
The rapid expansion of telehealth services brought myriad benefits

“When the COVID-19 pandemic started, health care providers rapidly transitioned to offering telehealth care to ensure that our patients could continue to be safely cared for while we navigated the uncertainty of the pandemic.
“This allowed our patients to manage logistics such as transportation, parking and time off from work to more efficiently get medical care from the safety of their own home, which was essential during the early stages of the pandemic. I have had many patients who were satisfied with their virtual experience, appreciated having that option to reduce their anxiety about leaving home early on and found it to be a valuable alternative to being seen in person.”
— Shalina Nair, MD, a physician in the Ohio State Wexner Medical Center’s Department of Family and Community Medicine and a clinical associate professor in the Ohio State College of Medicine
“Telemedicine in veterinary medicine, especially for re-check appointments, has given veterinarians a much better understanding about our pets’ home environments. This has been especially useful for cats.
“Purchasing equipment that’s facilitated having our students have a full view of patients and clients has also allowed us to have additional family members attend appointments virtually, allowing us to deliver one message without breaking social distancing precautions. In some situations, the lack of travel time is what really allowed the additional people or even a pet trainer to attend the visit remotely.”
— M. Leanne Lilly, DVM, a board-certified veterinary behaviorist and an assistant professor of Behavioral Medicine in the Ohio State College of Veterinary Medicine
“Being part of an organization that’s delivering care in a sustainable way is really exciting. Telemedicine has been around for years, but regulations governing where and how it could be used had long deterred both providers and patients.
“The sudden demand for virtual medical visits in early 2020 led to a rollback of restrictions and allowed us to really increase the number of telehealth appointments to many times that of pre-COVID-19 levels. For instance, there were 800 telehealth appointments in the first three quarters of fiscal year 2020 — but since March 2020, we’ve had nearly 740,000 telehealth visits!
“Some patients have to take multiple buses to get to our hospitals. Access to transportation should not be a constraint for getting care. Telehealth appointments have not only resulted in better access and higher patient satisfaction rates, but it also saved over 2 million gallons of gas for patients, avoided 24 tons of waste being generated and prevented over 16,000 metric tons of carbon dioxide emissions (equivalent to taking 3,480 cars off the road annually).
“We’ve had similar gains as a result of our flexible workplace policy, allowing eligible employees to work from home. The emissions from employee commutes in fiscal year 2021 were only half of the emissions of fiscal year 2020, saving 20,000 metric tons of CO2. It would take over 24,000 acres of U.S. forests to sequester that amount of carbon in one year.”
— Aparna Dial, MS, MBA, LEED AP, senior director of Sustainability and Strategic Services for The Ohio State University and the Ohio State Wexner Medical Center
“In the course of our research, we have had the opportunity to speak with a number of Ohio State primary care physicians about their experiences using telehealth during the pandemic. These physicians noted a number of positive aspects of delivering virtual care and reported being pleasantly surprised at how feasible it was for both their patients and themselves.
“The doctors we interviewed suggested that telehealth appeared to benefit patients in a number of ways, including providing an easy and convenient way to access care as well as the ability to quickly get needed specialty referrals. Physicians also commented that patients seemed profoundly grateful for the ability to receive high-quality care when in-person visits were not an option. Overall, physicians were reportedly encouraged by these experiences and optimistic about their ability to use telehealth for care delivery in the future.”
— Ann McAlearney, ScD, associate dean for Health Services Research at the Ohio State Wexner Medical Center and distinguished professor in the Department of Family and Community Medicine at the Ohio State College of Medicine
We improved our understanding of disease transmission and prevention

“I think that we’ve been able to help some people understand the interconnectedness of humans. Public health interventions come in many different forms. Sometimes, they are intended to protect only the person themselves. Other times, like with masks or vaccines, we’re trying to protect both the person receiving the vaccine or wearing the mask and the people around them. Sixty years ago, that was much more obvious to people.
“They understood the benefits of polio or measles vaccines and how getting it would help others as well as themselves. But when infectious diseases became less of an issue, the focus shifted completely to personal responsibility for one’s health. This pandemic has helped people see how their actions can affect others. And that’s a message that I hope even more people hear.
“I also think that people simply have a better understanding of public health, in general. Public health is not the same as medicine. They’re intimately related, of course, but public health is working at a community or population level, rather than an individual one. And in the past two decades, spending for public health has been drastically reduced. The pandemic may change that, at least in some places. If spending does increase, it will help us to reduce the impact of the next COVID-19-like event.”
— William Miller, MD, PhD, MPH, senior associate dean of Research and professor of Epidemiology in the Ohio State College of Public Health
Health care institutions and experts collaborated like never before, creating new pathways for sharing resources

“Health care coalitions and existing relationships were leveraged for the good of all patients. For example, OhioHealth helped Ohio State care for patients with COVID-19 during a surge of cases among prison inmates to help special populations during the pandemic. Mount Carmel sent us extra drugs, like monoclonal antibody treatments, when we had a higher volume of COVID-19 patients and had used up our supply.
“The central Ohio health systems also worked together on preparing potential alternate care sites, such as the Greater Columbus Convention Center. We also worked together to handle medication and supplies that were in extreme scarcity by comparing plans and tactics. This type of care coordination is necessary during disasters, and I hope this care coordination continues beyond the COVID-19 pandemic.”
— Nicholas Kman, MD, emergency medicine physician at the Ohio State Wexner Medical Center and a clinical professor in the Ohio State College of Medicine
“This pandemic has taught us how to work together in new ways across so many disciplines here at The Ohio State University and beyond: from physicians to veterinarians, virologists to epidemiologists, disease modelers to engineers, wildlife rehabilitators to hunters and environmental scientists to farmers. We saw people come together in amazing, unexpected and creative ways and use their skills, abilities and knowledge to address this pandemic — from treatment, to prevention, to surveillance for animal reservoirs — all in the name of protecting human, animal and environmental health, which, as this pandemic has reminded us, are inextricably linked.”
— Vanessa Hale, DVM, PhD, MAT, assistant professor in the Department of Veterinary Preventive Medicine at the Ohio State College of Veterinary Medicine
The standardization of mass testing and vaccination sites means we’re better prepared for future disasters and pandemics that need these tools

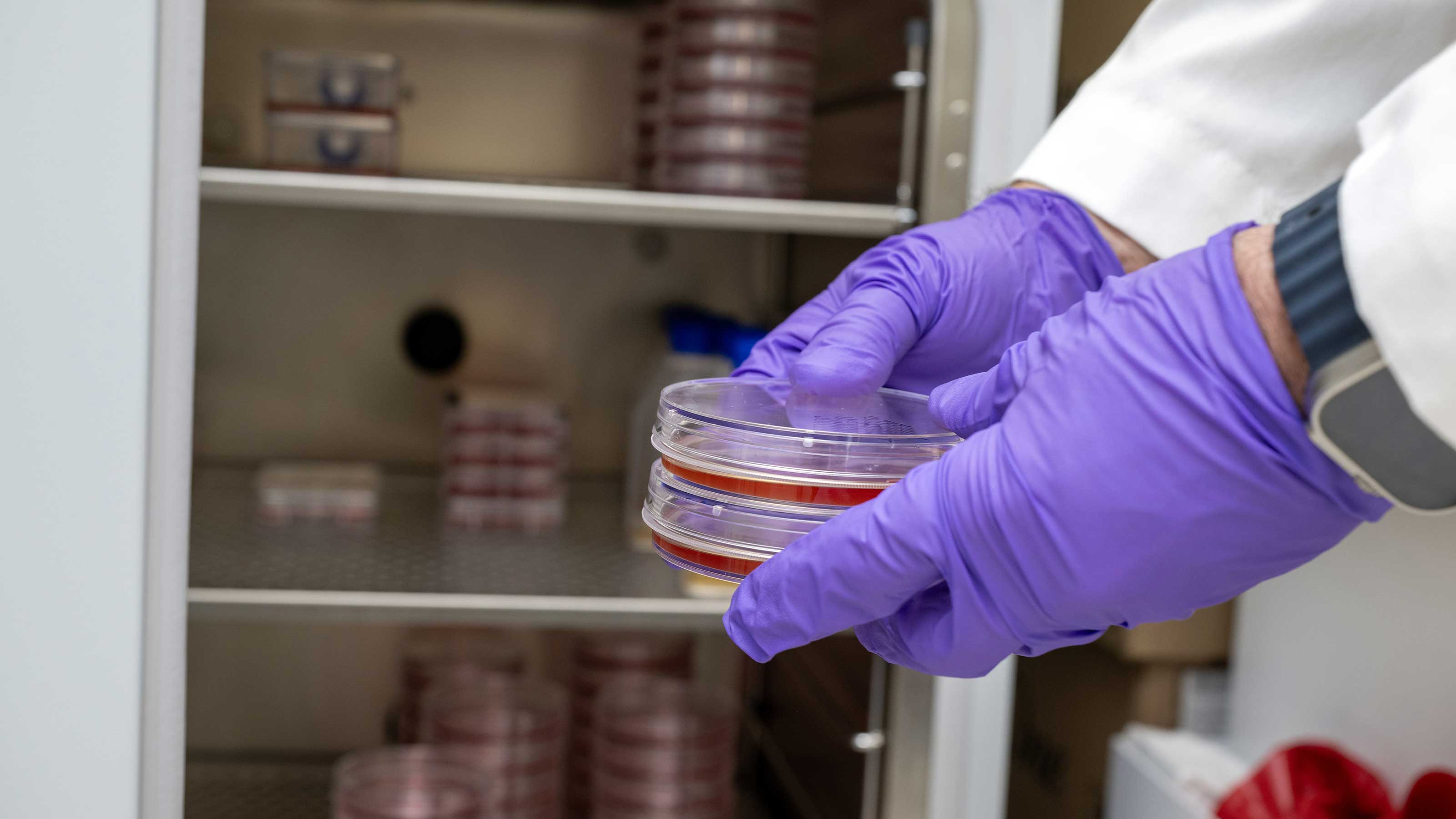
“Although COVID-19 started gradually, it quickly developed an aggressive trajectory with widespread impact throughout our society and world. Part of the initial response from the Ohio State Wexner Medical Center required the ability to test patients for the virus causing COVID-19.
“The testing had unique requirements from other previous types of tests done in the medical setting, including the ability to schedule the test with only indirect interaction between the patient and the health care provider, and the ability to perform the test in an open-air setting. The volume of patients being tested exploded quickly and required ongoing efforts to increase our capabilities for scheduling, collecting tests, performing the lab analysis and reporting results.
“A concerted multidisciplinary push from our staff allowed this response to succeed. At Ohio State, we benefited from collaboration across the university and community to provide swabbing supplies, testing platforms and PPE when standard supply chain resources were quickly exhausted. This combined operation made Ohio State a regional and statewide leader in the testing environment for COVID-19.”
— Daniel Bachmann, MD, an emergency medicine physician at the Ohio State Wexner Medical Center, a clinical associate professor in the Ohio State College of Medicine
Our disaster preparedness was effective, and what we learned readies us for a potential future event
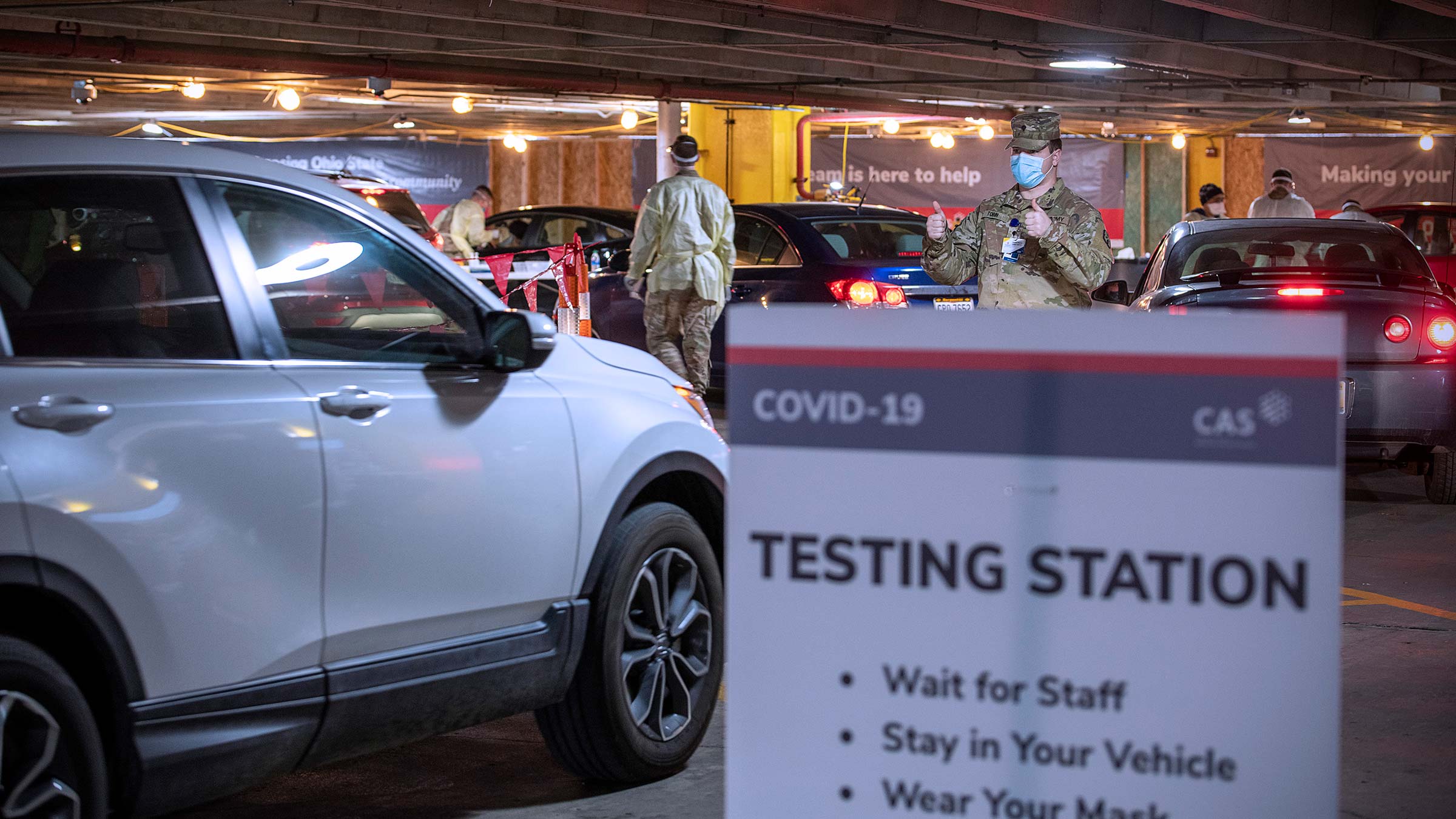
“The importance of disaster preparedness was on display during the early days of the COVID-19 pandemic. Central Ohio was well prepared, thanks in part to the work of organizations like the Central Ohio Trauma System (COTS) and the Columbus Metropolitan Medical Response System (CMMRS).
“When the supplies from the Strategic National Stockpile dried up, we were able to rely on supplies from the COTS’ Disaster and Personal Protective Equipment cache. This allowed us to distribute N100 masks and respirators more easily. I think this illustrates the importance of planning ahead for disasters, and resources hopefully will continue to be available for disaster response in the future so that we’ll have everything we need to respond appropriately.”
— Nicholas Kman, MD, emergency medicine physician at the Ohio State Wexner Medical Center, a clinical professor in the Ohio State College of Medicine and a disaster responder with Ohio Task Force 1, FEMA Urban Search and Rescue
“Throughout the pandemic, the role of the Contact Center that handles calls from patients and health care professionals shifted many times. We moved quickly to get our 200+ team members working from home within just two weeks. While getting used to communicating as a fully remote team, we supported our clinics and patients with the rapid shift of thousands of visits to telehealth.
“Throughout the pandemic, our team became the patient resource for all things COVID-19-related, including telehealth, immediate care options, transition of care clinics for COVID-19-positive patients, swabbing, vaccination and post-COVID-19 recovery. Despite the ever-changing landscape of care and changes to how our team functioned, we were able to continue to provide uninterrupted support to our patients.”
— Brooke Bellamy, MBOE, senior director of Access and Capacity Management, the Ohio State Wexner Medical Center
New legislation and regulations expanded access to care and better positioned many health care professionals to help patients

“Pharmacists across the country stepped up during the pandemic to quickly operationalize testing, vaccination and treatment of patients with COVID-19 and support their colleagues on the interprofessional health care team, while ensuring that patients continued to have access to and knowledge of their lifesaving medications.
“Decision-makers from state legislators to the president of the United States saw the potential in the pharmacist to provide vital services during the public health emergency and passed laws, regulations and executive orders to expand the profession’s ability to serve their communities.
“Although the pandemic has been stressful on all members of the health care team, a silver lining can be found in the result of these expansions in pharmacists’ ability. Now more than ever, a greater amount of the public, decision-makers and other members of the health care team have a stronger understanding of the role and value of pharmacist-provided care. It will be exciting to see the implementation of more changes on the horizon that continue to increase accessibility to high-quality, equitable and affordable health care.”
— E. Michael Murphy, PharmD, assistant professor of Clinical Pharmacy in the Ohio State College of Pharmacy and advisor for State Government Affairs at the American Pharmacists Association
Animal shelter procedures changed for the better

“The pandemic led to the development of a community-supported shelter model. This expanded the care of homeless animals beyond the walls of the shelter and into the community. Many lost pets stayed with their finder while the shelter assisted in locating their owner. Through foster programs, thousands of people temporarily welcomed shelter animals into their homes while they were waiting to be adopted.
“It’s great to know that shelters can expand their lifesaving efforts into the community. And the pets enjoy more spacious accommodations with lots of perks. Moving forward, many shelters plan to involve the community more as they help address pet homelessness together.
“Like everyone else, shelters had to dramatically alter their operations to reduce the spread of COVID-19. This meant reducing the number of people in the shelter and finding new ways to deliver services. Managed Intake and Managed Adoptions have been around for a while, but few shelters utilized these methods of scheduling appointments to receive animals being surrendered and for adopters looking for a new pet. The pandemic made these protocols a necessity and the results were really beneficial.
“Scheduling appointments allows shelters to know how many people will be there so that staff can be ready to provide the services they need. This means less waiting and more personal attention. Scheduling appointments allowed staff to help clients keep a pet they were surrendering for reasons that could be addressed by connecting them with the support they need, and to help new adopters find the best match in their new pet.
“Additionally, many shelters employed virtual appointments so that potential adopters could meet animals over live video and ask questions about them. Many adopters decided which pet they wanted before they even arrived at the shelter, which meant they spent less time in the shelter, further lowering COVID-19 risks for all.”
— Jeanette O’Quin, DVM, MPH, associate professor in the Department of Veterinary Preventive Medicine at the Ohio State College of Veterinary Medicine
We got better at observing our pets’ health

“People are observing their pets a lot more closely and more often. This means that clients may be more likely to see subtle signs of illness early, giving them a better prognosis. For example, hiding is a classic, nonspecific sign of illness in cats.
“If your cat is always ‘Zoom-bombing’ your work calls, it takes just a day of hiding during a few calls for the client to notice their cat is acting different. If that client were at work, hiding during the day could go unnoticed for a week or more.”
— M. Leanne Lilly, DVM, a board-certified veterinary behaviorist and an assistant professor of Behavioral Medicine in the Ohio State College of Veterinary Medicine
We’ve learned more about epidemiology and public health, and their roles in society

Epidemiology, or the study of diseases in populations, took center stage in the public eye with COVID-19. Google Trends show that searches for the field nearly doubled in March 2020 at the start of the pandemic. Here at Ohio State, the College of Public Health has seen a 10% increase in graduate applications for public health since 2020 and an increase of more than 40% in applications for its Master of Public Health degree in Epidemiology.
“I’m hoping that greater awareness of our field increases respect for it. And with greater awareness, we can have an opportunity to improve all kinds of health outcomes, not just for infectious diseases.
“I think we’ve learned a lot about how not to do things. And we’ve learned from those mistakes. We have learned that communication is so important. We’ve learned that vaccine hesitancy is complex and multifaceted.
“We’ve learned that many of our data collection systems are not as sophisticated as they need to be. But then we’ve learned to adapt and adjust quickly to get most of the data we need. And I’m hoping that we can use this knowledge to do better next time.”
— William Miller, MD, PhD, MPH, senior associate dean of Research and professor of Epidemiology in the Ohio State College of Public Health
Health care expanded further into the home, becoming more accessible for many
“At Ohio State during the pandemic, we significantly ramped up our home-based and post-acute care to meet patients where they are, and this will continue long-term. We’re continuing to build a more connected care continuum that extends beyond outpatient clinics, with The Ohio State University Wexner Medical Center Home Care, Ohio State Home Medical Equipment and stronger, more clinically integrated relationships with skilled nursing facilities, long-term acute care hospitals and hospice care facilities.”
— Rachit Thariani, chief administrative officer, Post-Acute and Home-Base Care Division, the Ohio State Wexner Medical Center
There’s now more support and acknowledgement for mental health in health care workers

“The pandemic has illuminated the emotional toll that working in health care can have on individuals, and it showed the need for full-spectrum support options for health care workers that are well publicized, easily accessible and stigma-free. Practically speaking, this means offering and promoting a variety of programs, some of which focus on preventive maintenance and resilience-building, and others that focus on intervention and mental health care.
“The goal is to create a systemwide culture of support and compassion that honors the difficult and important work health care workers perform every day, and that deploys the right resources to the right spaces at the right times to support the emotional health and overall well-being of staff.
“At the beginning of the pandemic, Ohio State was fortunate to be able to leverage the effort and expertise of programs that existed prior to this crisis to quickly erect support options for staff. For example, the Stress, Trauma And Resilience (STAR) program, which since 2009 has been offering training, support and care for health care providers facing difficult clinical situations, was able to operate a live support phone line staffed by specially trained clinicians who could offer peer support for staff who were coping with anger, uncertainty, exhaustion and fear.
“They expanded access to training in their Brief Emotional Support Teams model that teaches participants how to recognize the signs of stress or trauma, and how to intervene effectively with peers on their units who might be experiencing a crisis. They also developed daily coping tips that were paired with a short, light-hearted video to encourage staff to take a break for health self-care practices, and they published a webinar series where staff could learn additional coping skills.
“A twice-daily virtual support group was set up for staff who were feeling isolated because of social distancing requirements or the shift to working from home, and the team fast-tracked connections with mental health counseling for faculty and staff who would benefit from more formal support.”
— Arianna Galligher, LISW, associate director of the STAR Trauma Recovery Center at the Ohio State Wexner Medical Center
“We are experiencing a mental health pandemic exacerbated by the experience of the last two years. The rise in stress, anxiety, depression and burnout has also increased the volume of conversation and care surrounding the emotional and psychological impact of COVID-19. We are seeing more students seek out help and support resources, including the College of Nursing’s MINDSTRONG program, to learn cognitive-behavioral skills-building that increases coping and resilience.
“One student reflected the perspective of many in telling me, ‘There are some days that the techniques you taught me are helping me tremendously. I appreciate you and hope to get better in my life (both academic and personal) every day.’ Continuing to acknowledge and address our own psychological stresses will help us not only find balance in our own individual worlds, but also bring needed balance to a world whose crises weigh on us all.”
— Jacqueline Hoying, PhD, RN, NEA-BC, director of the MINDSTRONG program and an assistant professor of Clinical Nursing in the Ohio State College of Nursing
“One silver lining of the pandemic is the more consistent use of vitamin G for gratitude. People have really gotten into the consistent habit of taking and giving daily doses of vitamin G. It is a brief, evidence-based practice that reduces stress and blood pressure as well as improves mood and sleep. During Valentine’s Day week, our nursing students wrote gratitude cards with special appreciation to our frontline health care workers.
“With Buckeye Paws, Chief Clinical Officer Andy Thomas and I visited many clinical units to offer our gratitude and deliver these cards — this dose of vitamin G for our awesome staff was deeply appreciated. I’ve also witnessed more clinicians advising their patients to do the same thing. Try it and see the positive impact it makes!”
— Bernadette Mazurek Melnyk, PhD, APRN-CNP, vice president for Health Promotion and chief wellness officer for The Ohio State University, and dean and Helen Fuld Health Trust Professor of Evidence-Based Practice in the Ohio State College of Nursing

When you give to The Ohio State University Wexner Medical Center, you’re helping improve lives
We’re committed to making advancements in research, education and patient care that will have an impact throughout Ohio and the world.
Ways to Give