New hope for neurological disorders
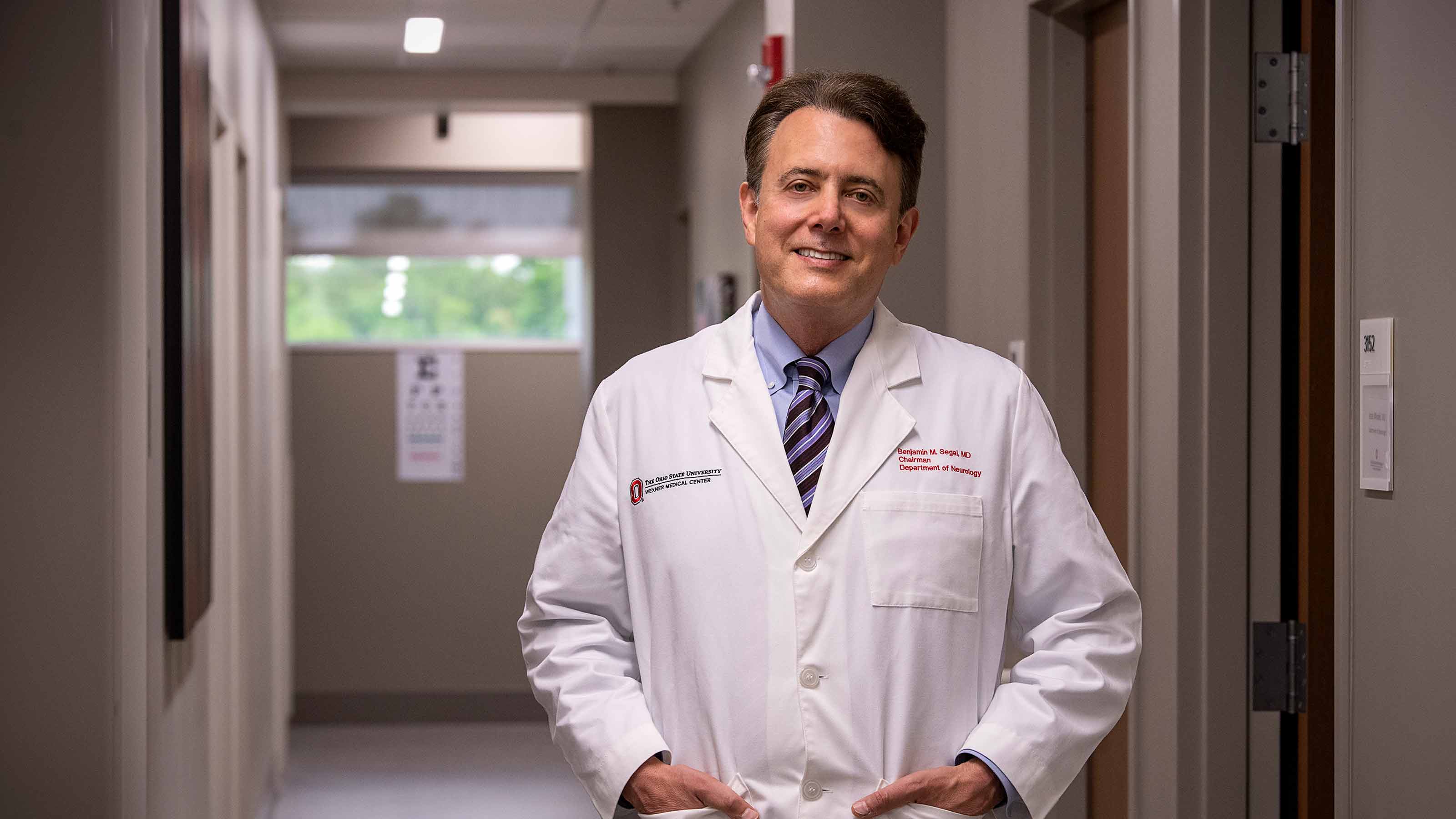
Ohio State neurologist Benjamin Segal, MD, is on the forefront of research that will not only slow the progression of neurological disorders, but also has the potential to reverse damage that has already been done.
For patients living with neurological disorders, there have been more than a few glimmers of hope over the past two decades. Biomedical researchers have developed new pharmaceuticals that suppress seizures in patients with epilepsy, treat symptoms of Parkinson’s disease, and even prevent the occurrence of multiple sclerosis (MS) episodes by up to 70% or more.
What these drugs and treatments have not been able to accomplish is to reverse damage that has already been done. Once lost, vision, strength and sensation are usually gone forever.
But there is hope. At The Ohio State University Wexner Medical Center, researchers are working to develop cutting-edge therapies that can drive repair of the central nervous system.
Several years ago, Benjamin Segal, MD, led a team that discovered a new type of immune cell with the potential to not only rescue damaged nerve cells from death, but also to stimulate the regrowth of severed nerve fibers. For millions living with MS and other neurological disorders, this research carries the promise of healing, not just survival.
A lasting impression
Dr. Segal, a neurologist who specializes in the diagnosis and treatment of MS and related disorders, joined the Ohio State Wexner Medical Center in 2019. He wears more than a few hats in his roles as chair of the Department of Neurology, director of the Neurological Research Institute, director of the Multiple Sclerosis and Neuroimmunology Center, and the Stanley D. and Joan H. Ross Chair of Neuromodulation in the Ohio State College of Medicine. He has been named a “Top Doctor” by Castle Connolly, received over $1.3 million in annual funding for research in MS and neuroimmunology, and received more awards than a bookshelf can hold.
But before the titles and the accolades, he was a kid in the Bronx with an ambition to become the first college graduate in his family. Dr. Segal traces his fascination with human physiology to his first high school course in biology. “I realized then that I wanted to pursue a career that was centered on understanding human health and disease,” he says. Looking back, it might have made more sense to pursue a PhD than an MD, he reflects, but he followed the advice of those around him to forge a path to medical school.
While earning an undergraduate degree and a medical degree from Brown University, Dr. Segal took a series of graduate-level courses in biomedical science.
“I was so fascinated with immunology, one of the subjects of these courses, that I began to think about becoming a physician-scientist,” Dr. Segal says. “But first, I resolved to become the best clinician I could.”
Benjamin Segal, MD (right, forefront) with members of The Segal Lab.
During his neurology rotation in medical school, Dr. Segal worked in close proximity to mentors who had mastered the skill of diagnosing neurology patients in what he calls a “refined art that involves plenty of deductive reasoning.” By the end of his rotation, he had charted a new course for his career. Determined to understand more about the cellular and molecular underpinnings of thought and emotion in the brain, he completed an internship in medicine at the University of Chicago before undertaking a neurology residency at the New York Hospital/Weill Cornell Medical Center.
The MS patients Dr. Segal encountered during his neurology residency left a lasting impression on him. “This is a disease that arises in young adulthood and persists for a lifetime, manifesting in countless ways that we had no way to treat at the time,” he says.
It was the early 1990s, and not a single therapeutic drug existed to lower the risk of MS attacks or alleviate the progression of the disease.
He vividly remembers Theresa, one of the very first patients he treated as a board-certified neurologist. In her occupation as a carpenter, Theresa began to notice diminished strength in her right hand when using tools, as well as a foot drop at the end of a long day of work. Most MS patients initially suffer from a form of the disease called relapsing-remitting MS, which manifests in periodic episodes that last for days or months until symptoms subside. Theresa had a rarer form called primary progressive MS, which results in steady, unrelenting decline that begins with the onset of symptoms and continues across a person’s lifespan. Within a few years, Theresa lost the use of her right hand and began using a cane. She had to retire prematurely.
Inspired to discover regenerative treatments for patients like Theresa, Dr. Segal immersed himself in biomedical science at the National Institutes of Health (NIH), which he joined in 1993.
Dr. Segal explains multiple sclerosis, its causes and the promise of immunotherapy to treat MS.
Laying the groundwork to change treatment for MS
At the NIH, Dr. Segal conducted research in multiple sclerosis and neuroimmunology that would lay the groundwork for his later breakthroughs. He was the lone MD in a sea of PhDs in his immunology lab, which suited him well. For six years, he immersed himself in basic science alongside some of the world’s most accomplished immunologists. “They didn’t hand out PhDs at NIH, but I put in the time to learn how to design experiments and interpret results,” he says. “This is where I became a bona fide scientist.”
Released in 1993, the first FDA-approved drug to treat MS symptoms decreased the risk of relapse by 25-30%, a stunning achievement at the time. Over the next two decades, Dr. Segal and his fellow researchers played a vital role in building off this success. In an endless pattern of trial and error, they identified the root causes of destructive inflammation, identified which immune cells should be targeted within the nervous system and partnered with pharmaceutical companies to initiate clinical trials.
Thanks in part to their dedication, more than 15 drugs now exist to treat MS, some of which decrease the risk of relapse by as much as 70% and higher. “People try to claim credit for certain drugs, but it really has been a global effort,” says Dr. Segal. Most of the drugs are geared toward patients with relapsing-remitting MS, but at least three drugs are approved to slow the progression in patients with progressive MS, like Theresa.
As a medical resident in the 1990s, Dr. Segal saw young MS patients who were likely to become significantly disabled within 15 to 20 years of their diagnosis. They typically started out with relapsing-remitting MS before moving into a progressive phase. Now, when these patients are diagnosed and treated expertly with MS drugs, they have a good chance of leading fully active lives.
While Dr. Segal has found tremendous satisfaction in being a part of a large-scale effort to improve MS treatment, it’s never been enough for him to prevent and treat damage. He aspired to modulate the immune system in a way that actually leads to healing and protection instead of inflicting injury to the nervous system.
And, for the past decade, that’s exactly what he has done.
A breakthrough for multiple sclerosis
In 2007, Dr. Segal was recruited to lead the University of Michigan’s Division of Multiple Sclerosis and Neuroimmunology. While he achieved great success in preventing and alleviating symptoms on the clinical side, the most groundbreaking developments were happening behind the scenes in the Segal Lab.
In general, the central nervous system is less resilient and more resistant to repair than other organs. Once severed and damaged, nerve fibers within the central nervous system typically do not regrow. For many years, researchers have been exploring potential avenues for nerve regeneration by crushing the optic nerve in an animal model and experimenting with injecting growth factors into the back of the eye to spark regrowth.
At the University of Michigan, Dr. Segal became aware of a series of papers in which scientists had injected a fungal cell wall extract into the back of the eye and triggered an inflammatory response that was associated with the regeneration of nerve fibers down the optic nerve. Although this research dated back decades, the type of inflammatory cell that was driving the nerve regrowth had not been identified, and no one knew how it all worked. That’s where the Segal Lab came in.
Dr. Segal and his team analyzed the immune cells that accumulated in the back of the eye after the injection of the fungal cell extract. They successfully identified the specific molecule within the fungal cell extract that was triggering the immune response.
Then they discovered something completely unexpected: a new type of immune cell with neuroregenerative properties. While it resembles an immature neutrophil, a common type of white blood cell that helps the body fight off infection, it is unique in its ability to drive central nervous system regrowth. Through releasing growth factors — naturally occurring proteins or hormones that stimulate wound healing — these cells have the potential to increase the number of surviving nerve cells following an injury, and even stimulate the regeneration of broken nerve fibers.
Dr. Andrew Sas (right) says that Dr. Segal has a passion for raising up the next generation of researchers.
During his neurology residency at the University of Michigan, and later as a faculty member at Ohio State Wexner Medical Center, Andrew Sas, MD, PhD, was part of the research team that discovered the new cell type and published its findings in a landmark 2020 paper in Nature Immunology. “So many things that happen in a lab are not reproducible,” Dr. Sas says. “It was exciting to realize that our finding held up, and even more exciting to think about how to translate it for the benefit of human patients.”
In 2019, Dr. Segal moved to Columbus, Ohio, to join the Ohio State Wexner Medical Center as chair of the Department of Neurology. “I never aspired to be the chair of a department,” he says. “I’ve always been more focused on clinical and research excellence than administrative responsibilities. What drew me to the role was this tremendous commitment and growth that was happening at Ohio State in terms of the academic mission and innovative translational research.”
Soon after arriving, Dr. Segal established a 12-person lab that devotes a considerable amount of time to investigating the therapeutic potential of newly discovered, pro-regenerative immune cells for treating optic nerve damage, stroke, progressive MS, traumatic spinal cord injury and other neurological disorders.
He and his colleagues are also developing methods to trigger the differentiation of neuroprotective and pro-regenerative immune cells from bone marrow cells in the laboratory. In the long term, the goal is to be able to remove human bone marrow cells and trigger them to acquire regenerative, nerve-protective properties in a dish, before re-infusing these cells into patients with neurological conditions. Another strategy is to develop new pharmaceutical agents or gene therapies based on the reparative factors produced by the beneficial immune cells. By doing so, the Segal Lab aims to stimulate enough repair in the central nervous system to allow patients to reclaim lost functions and skills.
Unanswered questions abound: What is happening in the environment that drives the development of these unique immune cells that can potentially be simulated in people with neurological conditions? How can researchers engineer immune cells to become even more effective at healing? What other cell-based treatments carry the most therapeutic potential?
And that is just one line of research. The Segal Lab is currently investigating a broader range of questions with direct implications for MS patients, including the potential of the immune system to initiate disease remission or repair the central nervous system after a traumatic brain injury.
A community of healers
Recognizing that the need for translational research far exceeds the capacity of his own lab, Dr. Segal is an avid champion of other researchers, both within the Ohio State Wexner Medical Center and on a larger scale.
Currently, he serves as a director of the Americas Committee for Treatment and Research in Multiple Sclerosis (ACTRIMS). He originated and oversees the ACTRIMS annual Neurology Resident Summit and the annual Young Scientist Summit, two venues for young physicians and scientists to connect with peers and mentors and learn about the latest developments in multiple sclerosis diagnosis and treatment. According to Dr. Segal, an encouraging sign that these summits and events are worth the investment of time and energy is that the number of neurology residents who have applied to MS fellowship programs has tripled in recent years.
Dr. Sas, who followed Dr. Segal to Ohio State from the University of Michigan, says that Dr. Segal’s passion for raising up the next generation of researchers is evident in the relationships he builds. “As a mentor, he wants to see people rise,” says Dr. Sas. “He is known for being straightforward, direct and supportive in helping others make a plan for success and carry it out.”
“It’s easy to work for someone like him,” adds Erica Bell, PhD, who works with Dr. Segal as the associate director of the Neuroscience Research Institute. “He shows up to every lab meeting and meets with staff members on a regular basis, which is rare in his position. And, at the same time, he provides autonomy, which benefits us all.”
Dr. Segal speaks with pride about the members of his department, as well as his former trainees who are now professors at academic medical centers, prominent community neurologists, and physician-scientists in industry labs.

“It’s an honor to train people who will carry the baton forward and will be the first to discover new strategies for alleviating and reversing neurological disease,” Dr. Segal says.
This growing, global team of multiple sclerosis researchers and clinicians have experienced the frustration of watching patients suffer and decline, but they have also experienced once-in-a-lifetime discoveries.
“As a clinician, we often treat MS patients throughout their lives,” says Dr. Segal. “I have patients who still come to see me from the time I treated them in New York or Ann Arbor. There is this bond that forms. It’s an incredible privilege to use our knowledge and experience to help people with neurological diseases face and overcome challenges. And, step by step, we are moving closer to breakthroughs that can change the course of their lives.”

Ohio State's Neurological Institute
Pioneering discovery and expert care for neurological disorders
Read more