Ladies, your relationship with your breasts can save your life.
If you’re one of the many women with dense breast tissue, you’ll need to get extra familiar with your breasts in monthly self-exams. That’s because dense tissue can feel fibrous or lumpy compared with fattier tissue, and detecting an abnormal spot can be trickier.
Dense breast tissue is normal and common
Some women are surprised to find out they have dense breast tissue when notified after a baseline mammogram.
Screening mammograms are recommended to begin at age 40 and be performed annually along with a clinical breast exam by your provider. The law requires doctors to notify women of dense breast tissue.
But don’t stress. Having dense breasts is normal and common. If you learn that you have dense breasts after a baseline screening, it doesn’t mean you’ll have breast cancer.
It means you should start a conversation with your primary care provider to learn about all your risks and how you can begin monitoring for those risks.
Why it’s important to monitor for breast changes
What is dense breast tissue? And what does it mean if you have it?
Test your knowledge with our true-or-false quiz.
1 True or false? Half of women have dense breast tissue.
True.
High breast density is common. About 50% to 60% of women ages 40 to 44 have dense breasts.
Breast density varies greatly by age and weight, though. Dense breasts are more common in both young and thin women. Many factors can cause dense breast tissue, including genetics, age, having children, having a low body-mass index and using a post-menopausal hormone replacement therapy.
2 True or False? Dense breast tissue means your breasts are heavy.
False.
Density refers to the appearance of your breast tissue on a mammogram – not the actual weight of your breasts. Your breasts contain milk glands, milk ducts and connective tissue – those are all dense breast tissue. The rest of the breast is made up of fatty tissue, which is the non-dense part. So, if you have dense breasts, you have more glands, ducts and connective tissue than fat.
Dense breast tissue appears white on a mammogram. Non-dense tissue appears transparent (darker part in the image).
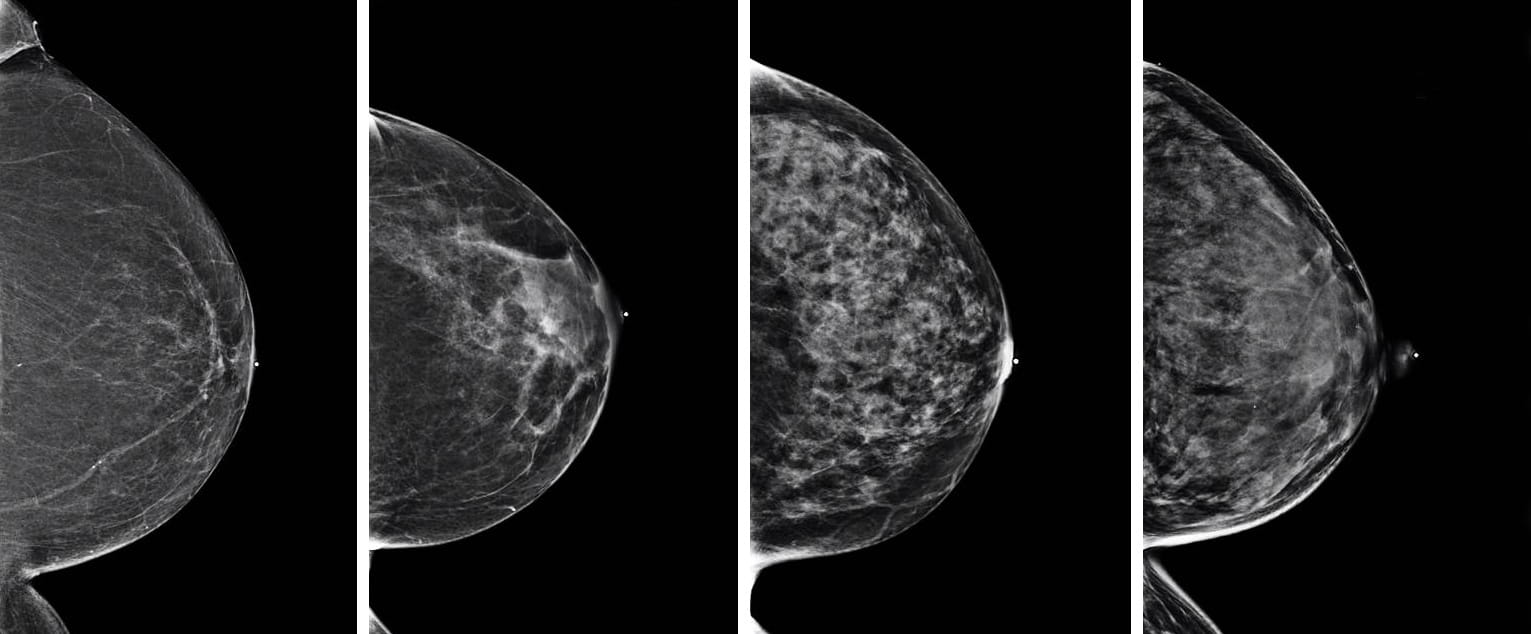
Cancer also appears white on a mammogram. Dense breast tissue is difficult to see through and could hide or mask cancerous growths.
3 True or false? Older women have denser breasts.
False.
Premenopausal women are more likely to have dense breasts. During menopause, milk glands and ducts diminish, leaving fattier, or non-dense, tissue.
Some of us, though, may continue to have dense breasts as we age, due to genetics or hormone therapy.
Density also can fluctuate over time, because of multiple different factors. It’s not uncommon to receive a letter saying you have dense breasts one year and the next year to not receive a dense-breasts letter.
4 True or false? The more weight you gain, the denser your breasts become.
False.
The opposite is true. The less you weigh, the denser your breasts become. That’s because the more weight you put on, the fattier your breasts become.
Why men should be tested for the breast cancer BRCA gene too
5 True or false? Having denser breasts increases your risk of cancer.
True.
Having dense breast tissue is a risk factor for cancer, although a small risk factor. However, it’s important to know so you can consider it with other breast cancer risk factors.
For women with dense breasts, an annual screening mammogram is the primary screening exam to identify breast cancer. However, there also are secondary screening tests to complement the screening mammogram, which also increase the number of breast cancers we can identify in dense breast tissue.
Screening whole breast ultrasound is one of these supplemental screening tests and is good for low- to intermediate-risk women with dense breast tissue. If a woman is found to have a high risk for breast cancer (>20%) then magnetic resonance imaging (MRI) of the breasts is recommended for supplemental screening. Therefore, it’s so important to discuss your risk factors with your primary care provider.
If you and your provider are concerned that you may fall in the high-risk category, you should make an appointment with one of our high-risk providers for further in-depth discussion of your risk factors and possible genetic testing.
How breastfeeding or pregnancy changes breast tissue
6 True or false? You may require follow-up testing if you have dense breasts.
True.
Having dense breast tissue makes cancer more difficult to see on a mammogram. Try to view the follow-up tests as a positive, because the No. 1 way to combat cancer is through early detection.
7 True or false? A mammogram is the only screen for breast cancer.
False.
Mammography is the first line for screening for all women over 40 years of age as it's been proven to find breast cancer early and decrease mortality from breast cancer. Currently, mammograms can be done in 2D or by using a technology called tomosynthesis that delivers 3D images. A tomosynthesis screening uses multiple images to create a 3D image that allows the radiologist to see areas hidden behind dense breast tissue. All mammogram machines are equipped with tomosynthesis at The Ohio State University Comprehensive Cancer Center – Arthur G. James Cancer Hospital and Richard J. Solove Research Institute, allowing us to offer all patients screening with 3D.
Supplemental screenings are available when a patient has dense breast tissue. Check your insurance plan to find out what supplemental screening exams it may cover, such as whole breast screening ultrasound or MRI.

Early detection saves lives
Schedule your mammogram with the experts at The James, who understand there is no such thing as a routine mammogram.
Schedule Now