
You might hear about your risk of ovarian cancer through an aunt, mother, sister or grandmother. For some, there are no signs of hereditary cancer in the family, but genetic testing still reveals a high hereditary risk.
Genetic testing could prevent you from ever having ovarian cancer.
“The only way to do that is to offer testing to people before they’ve developed cancer,” says genetic counselor Leigha Senter, MS.
Two genes, BRCA1 and BRCA2, are associated with several different kinds of hereditary cancer risk.
The two most predominant cancers we see in people with mutations in these genes are breast cancer and ovarian cancers, but the genes can also pose a hereditary risk for prostate and pancreatic cancers and even some melanomas.
“These genes really do cause a spectrum of cancer risk,” Senter says. “If we offer people BRCA testing, we could identify those at high risk who didn't otherwise know.”
There are a few factors to consider before genetic testing, including your family history, how it could affect your insurance, and how it might be useful to you.
It’s not always clear who’s at risk for ovarian cancer
For Brooke Lane, one of the first indications that she had ovarian cancer was a dull abdominal pain.
Eventually, that pain became so great she made a trip to the emergency department.
A CT scan later showed two large tumors on her ovaries. Her diagnosis was Stage 3 ovarian cancer.
 “The only thing worse than having cancer is not knowing you have it,” Brooke says recalling her 2018 diagnosis.
“The only thing worse than having cancer is not knowing you have it,” Brooke says recalling her 2018 diagnosis.
Her maternal grandmother died of colon cancer and she had no other family history of cancer.
Senter, her genetic counselor, recommended that Brooke undergo genetic testing, which identified a BRCA mutation.
Once the gene was identified, Brooke’s extended family, including her 63-year-old mother, Sharon, were tested for BRCA mutations.
“It’s complicated information,” Senter says, “while people often report that they are grateful to receive information about their family members’ positive genetic test result. It gives them a piece of information that could keep them healthy.”
Sharon also tested positive for the mutation.
For people who test positive and still have fallopian tubes and ovaries, it’s recommended to have the fallopian tubes and ovaries removed in their 40s.
Sharon was already at the age when ovarian cancer can start to develop. She underwent what was supposed to be preventive surgery. Surgeons found very early-stage ovarian cancer.

“Brooke’s diagnosis and decision to get genetic testing saved my life,” Sharon says.
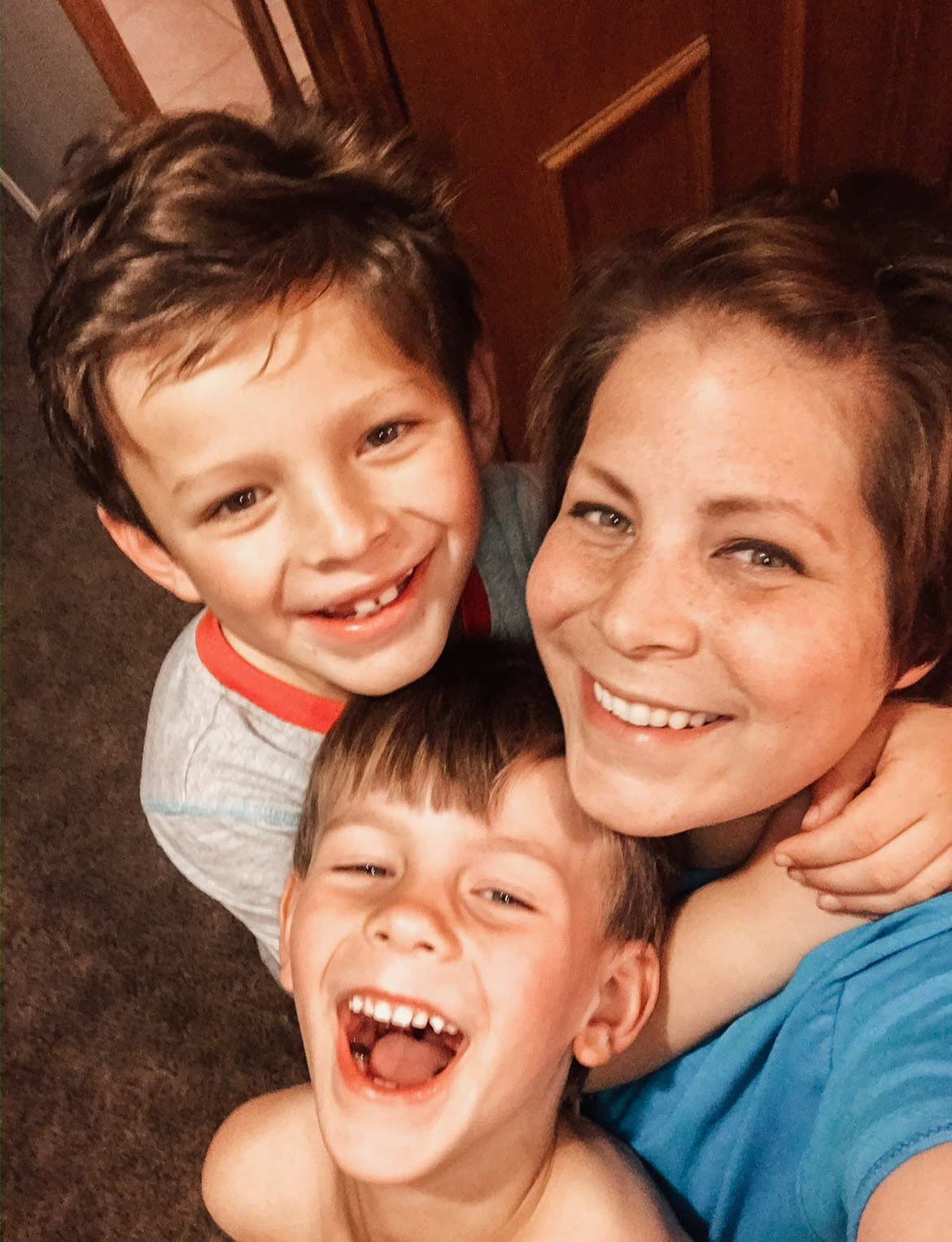
Brooke and Sharon underwent chemotherapy treatments together at the OSUCCC – James.
“It is a way we bonded that I could have never imagined going through,” Brooke says.
Who typically gets tested for BRCA genes?
- Anyone who receives a breast cancer, ovarian cancer or pancreatic cancer diagnosis
- Close relatives of people diagnosed with ovarian, pancreatic or breast cancers
However, family histories are sometimes vague or unknown. For example, if you have a distant relative who may have died from ovarian cancer, should you still consider getting tested?
“That’s where the importance of genetic counseling comes in. We can take into account all of those finer details, which every family has, and say, ‘Maybe we don't just check all of the boxes, but it would be reasonable to test,’” Senter says.
More genetic testing could mean fewer cancer cases, more lives saved
 The idea of offering genetic testing broadly could have huge implications for families like Brooke and Sharon’s, which had no previous history of ovarian cancer.
The idea of offering genetic testing broadly could have huge implications for families like Brooke and Sharon’s, which had no previous history of ovarian cancer.
“Ovarian cancer is a silent, devastating killer,” Sharon says. “I encourage every woman — and man — to understand their risk for inherited cancer for yourself, your kids, your grandparents, siblings, aunts, uncles and parents.”
Brooke recently had a cancerous place on her liver removed and is undergoing chemotherapy. Sharon continues to do well and shows no evidence of cancer.
Genetic testing factors to consider
- Identify first-degree and second-degree relatives you have and determine if any of them have ever had cancer. If so, what type?
- Talk to your doctor if you have concerns about risks for ovarian or other types of cancer. Ask if cancer genetic testing would be a reasonable consideration for you.
- Insurance often covers genetic testing. However, even without coverage, there are financial assistance options for people who are uninsured or underinsured, Senter says.
- If you think genetic testing might be useful to you, make an appointment with a genetic counselor. In most cases, a physician’s referral is not needed. “We can review what the options are for genetic testing and the pros and cons of each approach. Then you can make some decisions,” Senter says.
When to consider re-testing?
BRCA1 and BRCA2 are the most common causes of hereditary ovarian cancers. They’re not the only ones.
When undergoing genetic testing for cancer, more genes are now included.
“If a person had testing for just BRCA1 and BRCA2 in the past, they need updated genetic testing to include these more recently discovered genes,” Senter says.

Interested in speaking with an Ohio State genetic counselor?
Call 1-888-329-1654 with questions or click below for more info.
Genetic counseling at The James




