A ‘super’ way to ease fear, anxiety for pediatric radiation oncology patients
Radiation therapist designs custom superhero masks for children undergoing radiation therapy.
When children undergo radiation oncology treatment for pediatric cancers, they often feel vulnerable and anxious as they enter the strange, loud machine that will deliver their treatment. Making those kids feel invincible — brave in the face of repeated treatments — comes with the aid of a heroic radiation therapist at The Ohio State University Comprehensive Cancer Center – Arthur G. James Cancer Hospital and Richard J. Solove Research Institute (OSUCCC – James).
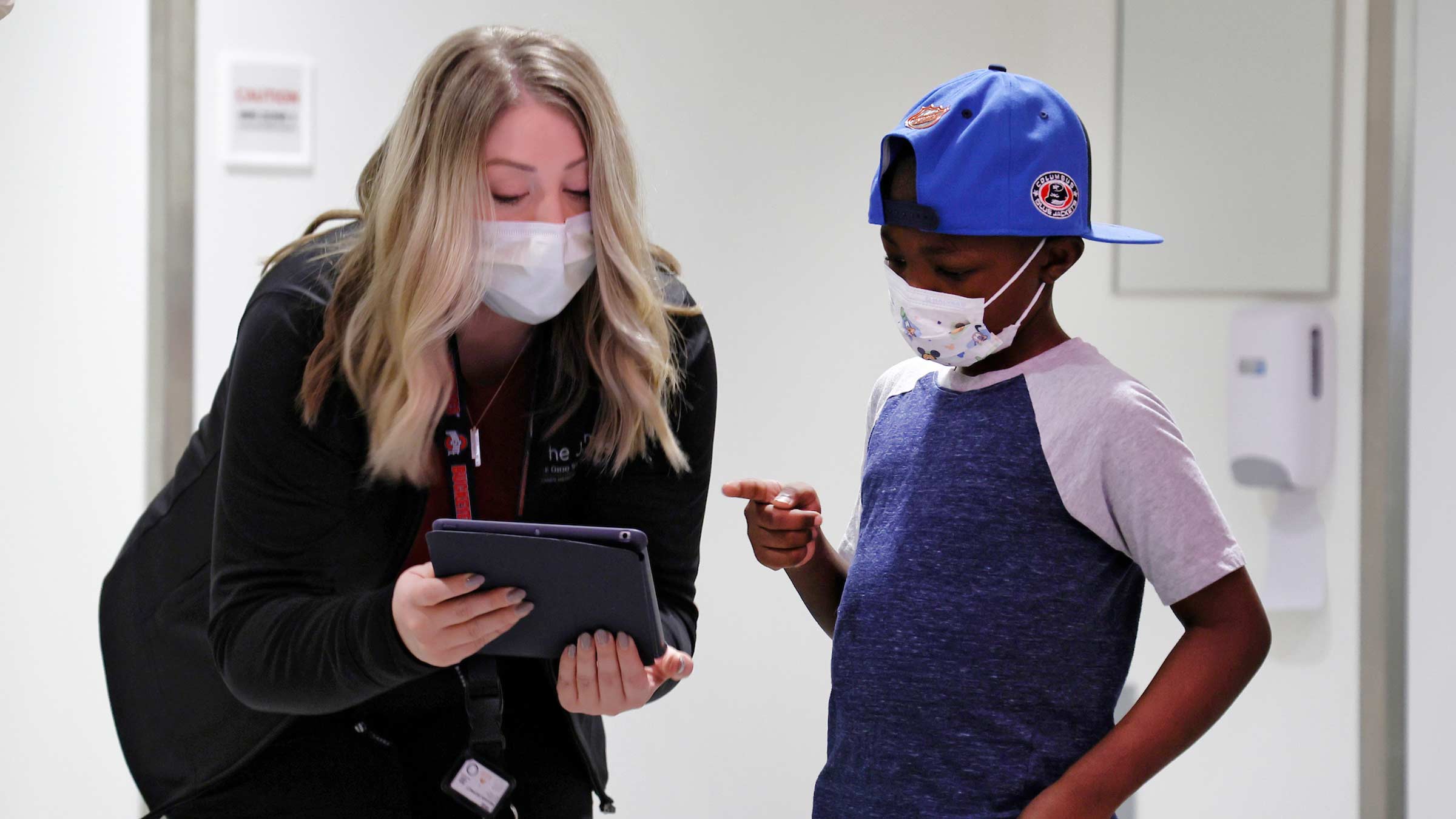
Jayceon McQuay, 9, of Fort Wayne, Indiana, recently took on the persona of Vegeta, the prince of a demolished planet in the fantasy game Dragon Ball Z, with the help of a custom superhero mask created by Julie Banner, a veteran radiation therapist of more than 27 years. Jayceon also recently completed a month of radiation therapy for a high-risk brain tumor at The James Cancer Hospital and Solove Research Institute. His treatment was part of an experimental clinical trial led by Nationwide Children’s Hospital.
When asked how the mask makes him feel when he puts it on, Jayceon replies, “Strong, brave, not afraid.”

A ‘heroic’ idea to reduce fear and anxiety for pediatric radiation therapy patients
Every patient who undergoes radiation has a treatment planning visit — known as simulation — where therapists position patients and make accommodations to ensure treatment can be delivered accurately and comfortably for the patient.
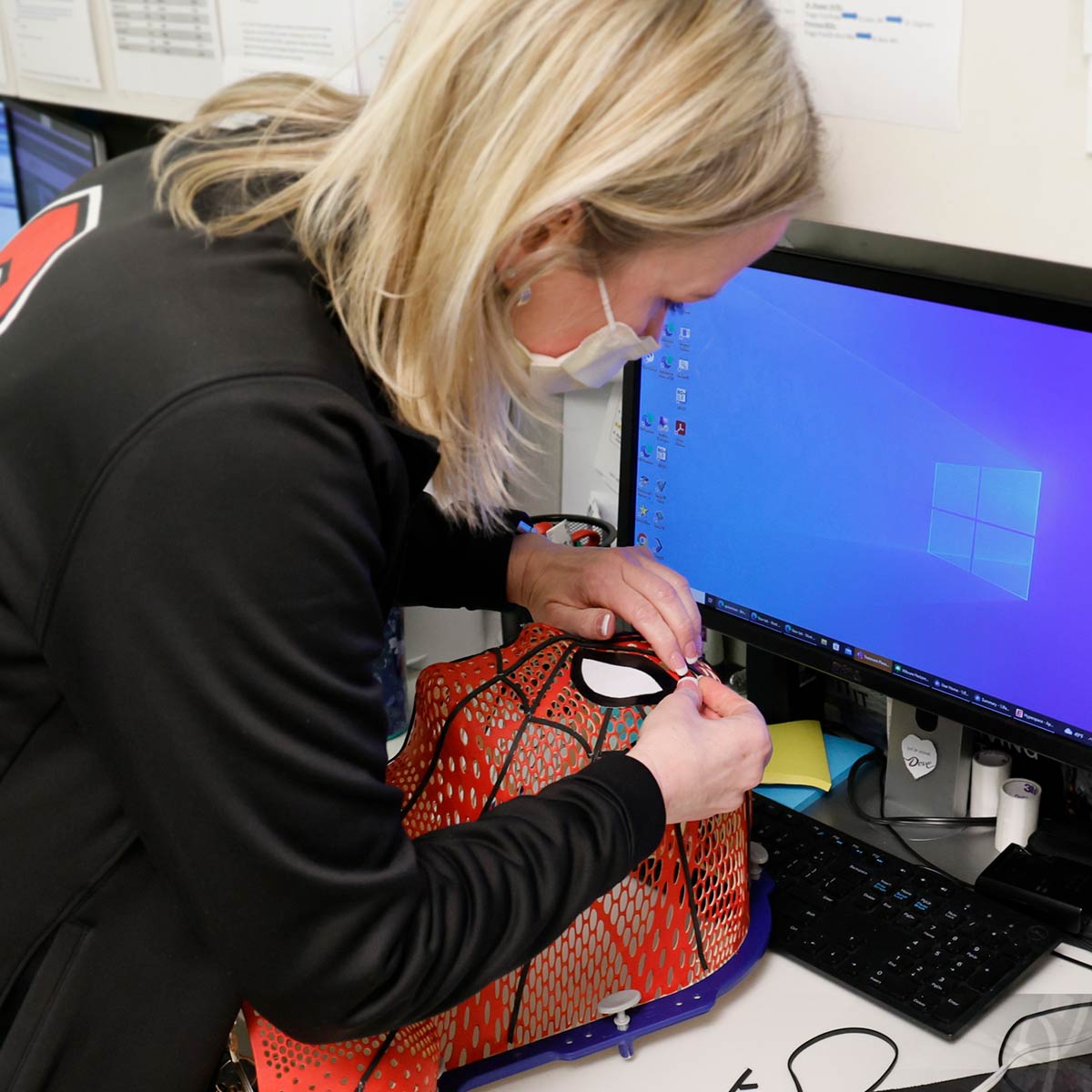
Banner is the lead therapist for simulation-planning appointments. When she saw children struggling with fear and anxiety about repeated radiation therapy treatments, she had an idea. What if she made a superhero mask — whatever character the child related to — for the child to wear throughout the course of treatment?
She researched materials, worked with radiation physicists to determine what could safely go into the treatment machine and began offering this to pediatric patients. Since then, she’s spent hundreds of hours — often on weekends and evenings — and her personal money to create custom masks for these patients.
Joshua Palmer, MD, head of pediatric at the OSUCCC – James, says radiation treatment can be challenging and scary for patients of all ages, but it is especially challenging for children who are faced with many unknown factors that can cause stress: new people, new environments, medical equipment and strange sounds.
He says the superhero masks have helped comfort pediatric patients — both through the distraction of the mask and by creating a familiar environment that makes the daily burden of radiation less intimidating.
“The kids really become the character, and that is a welcome distraction and comfort. Julie creates these masks in her free time and with her own money. I think that says so much about the level of connection our staff has with patients, and I am just extremely proud and grateful to work with people who care about our patients so much,” says Dr. Palmer.
“I just want to bring the children joy during a very hard and stressful time.”
— Julie Banner
“I meet them once in treatment planning and then rarely see them again,” Banner says. “Making the mask brings me joy because it is my gift to them. I hope in some small way it helps them feel cared for and safe when going through treatment.”
You’d expect that her clever crafting skills stem from a background in art — but they don’t. In fact, she says she has never been an artistic person. Her creativity comes from her job as a lead radiation therapist for treatment planning (simulation) appointments, where she is often challenged to use various materials to customize positioning supports. This requires ingenuity and creativity for some patients who may have altered or missing body parts due to cancer.
Banner has carried those skills into what she now considers her “job duties otherwise assigned” of superhero mask-making, though she does it happily as an act of service to others. Her most memorable and challenging mask? A 3-D Goofy face.

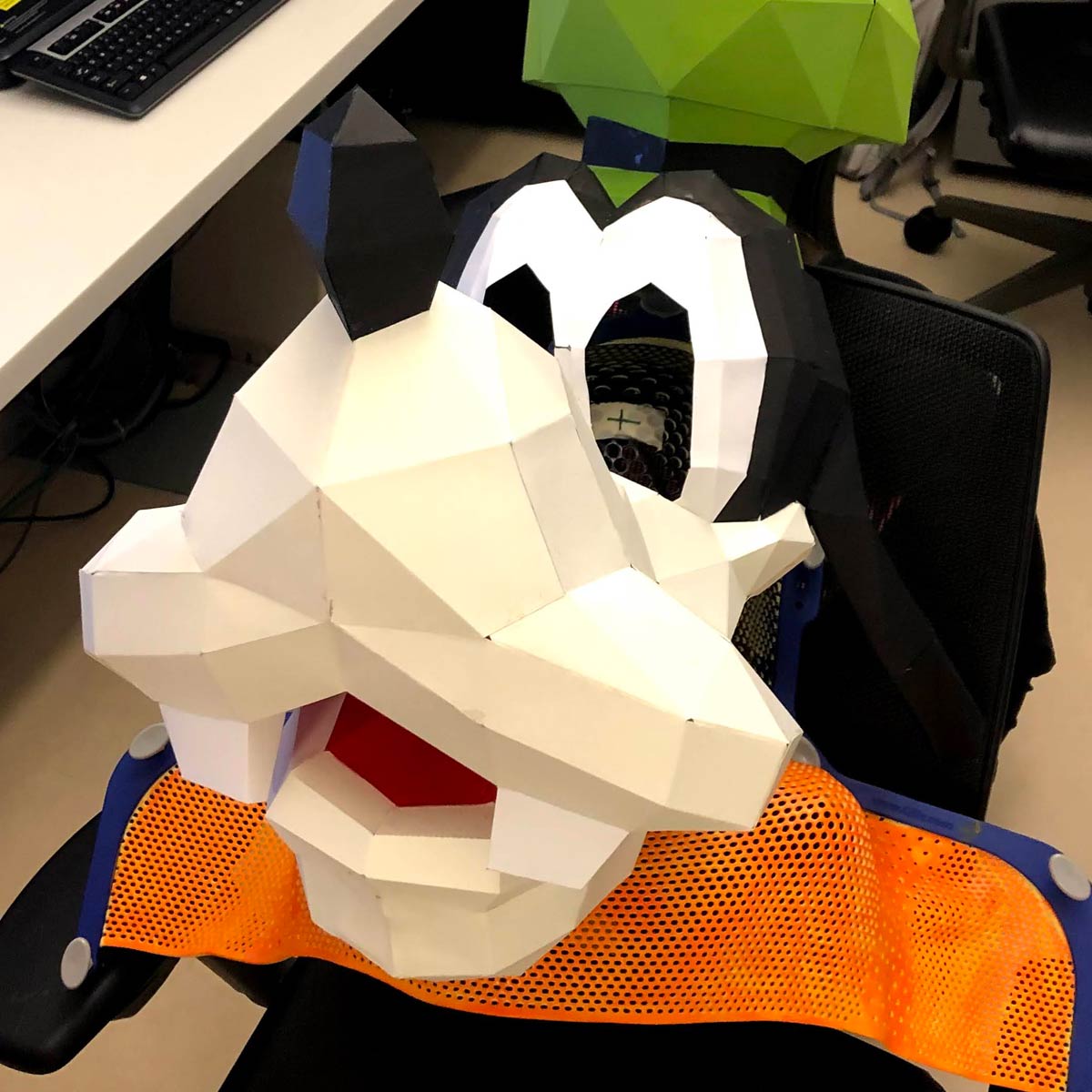

“That mask was an especially proud and memorable moment because it was for an older child, and it was technically very challenging. I spent 30 hours creating it,” she recalls.
She has since made a variety of characters, including Elsa, Avenger characters, a unicorn, a football player, a sunflower, animals, a pirate, Hermione Granger and a replica of a patient’s own dog.
Jayceon’s parents say the mask helped him feel brave, and they could see the characteristics of the character he chose in their son.
“My baby, he's very strong, he's passionate. He's stronger than any of us. Our baby's a fighter. He's a warrior. He's a survivor. Every day is a process, and he's walking through that process,” says his mother, Shaniqual McQuay.
Testing a new approach to improve pediatric radiation comfort and safety by reducing sedation
Kids are typically sedated for radiation treatment to limit movement and ensure accurate treatment delivery. Doctors are concerned, however, about the long-term impact on brain development from repeated sedation. Because of this, Dr. Palmer’s team conducted a clinical research study in partnership with Stanford University using a video streaming system known as AVATAR (Audio-Visual Assisted Therapeutic Ambience in Radiation Therapy) instead of general anesthesia in patients ages 3 to 10.
For this multi-institutional study, videos — for example, a child’s favorite movie — are shown from inside the radiation treatment vault as a distraction tool. At Ohio State, Dr. Palmer estimates that over 90% of patients who have tried the device have been able to complete treatment without sedation.
“It's been a huge success for us, and something we think will not only help the patients that we serve, but help patients throughout the world get better care, be more comfortable when receiving that care and use less anesthesia,” Palmer says.
The team reported the first successful treatment using this system to avoid general anesthesia in a 2-year-old patient with stage 4 Wilms tumor who required bilateral whole-lung and left-flank irradiation. The results of this case report were published in the May/June 2022 issue of Practical Radiation Oncology. Full results from this prospective clinical research study are expected in fall 2023.

Transforming the way cancers are detected and treated
Learn about the specialized treatments and clinics available at The James Cancer Hospital
Learn more




