Surgeon’s ‘MacGyver’ mindset brings customized solutions to patients with rare bone cancers
Joel Mayerson, MD, uses ingenuity to get results, find research funding for sarcomas.
If you ask surgeon Joel Mayerson, MD, why he never gives up when searching for solutions to even the toughest challenges facing his cancer patients, he might mention a TV show that first gained popularity in the 1980s.
“I just don’t accept no for an answer. There’s always a way to figure something out or to ‘MacGyver’ something,” says the orthopedic oncologist who specializes in removing and replacing limbs or portions of bones that have cancerous tumors. “If somebody hasn’t thought of it, that doesn’t mean you can’t think of a new way.”
Dr. Mayerson’s problem-solving materials are a far cry from the duct tape, Swiss Army knife or paper clips that might have been used by the fictional agent Angus MacGyver to troubleshoot his way out of various dilemmas. While the surgeon’s patients often inspire the same creative thinking and custom-made solutions, Dr. Mayerson’s tool kit is much more high tech.
Think 3D printing. Think artificial arms and legs controlled by the brain. Think machines that can tell the difference between cancerous and healthy tissue. Think the stuff that was science fiction on ‘80s television screens.
Now, they’re the newest tools of the trade that Dr. Mayerson uses as medical director of the sarcoma program and head of musculoskeletal oncology at The Ohio State University Comprehensive Cancer Center – Arthur G. James Cancer Hospital and Richard J. Solove Research Institute.
Building a sarcoma program to treat rare bone and tissue cancers
Sarcomas are cancers that affect bones, surrounding tissue and connective tissue, such as muscles, blood vessels and nerves. There are more than 80 types, and they’re rare — the National Cancer Institute estimates that bone and soft tissue cancers combined made up fewer than 1% of all new cancers in 2023.
That accounts for just about 17,000 patients, and it’s unusual for a cancer center to have a dedicated team focused on treating them. But Dr. Mayerson became a champion of such patients when he was hired in 2001.
Under his leadership, the sarcoma program has grown into a team that boasts 19 experts, draws patients from across the country and world, offers multiple clinical trials and gains interest from foreign surgeons seeking training.
Doctors are not always drawn to specialize in rare diseases that receive little research funding, but Dr. Mayerson’s commitment to creating an advanced program has helped attract top specialists to Ohio State’s Comprehensive Cancer Center – James Cancer Hospital and Solove Research Institute.
“He’s not afraid to be at that cutting edge. He’s always been interested in working with researchers and collaborating to push the boundaries to help his patients.”David Liebner, MD, the first medical oncologist to specialize in sarcoma at the OSUCCC – James, recruited to Dr. Mayerson’s program in 2013.
“He’s certainly excellent at what he does, but he doesn’t want to just be excellent,” Dr. Liebner says. “He always wants to look at whether we can push things a little bit harder.”

Maintaining quality of life
That tendency to push has led to some pretty cool procedures that are helping his patients.
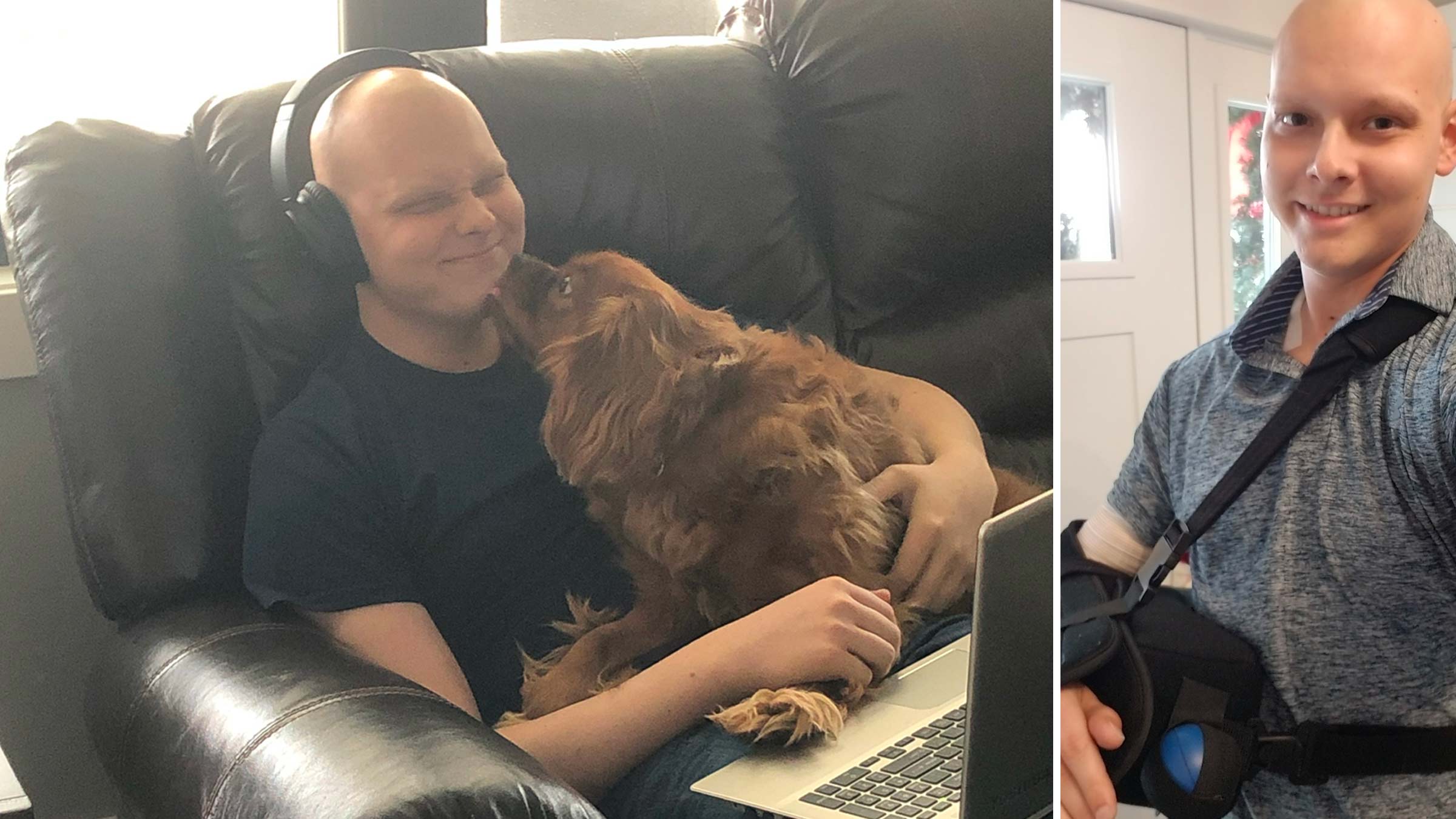
Chris Shultz, a data analyst from Atlanta, was 26 and living in Cincinnati when he benefited from Dr. Mayerson’s way of thinking.
His Ewing’s sarcoma diagnosis meant he’d undergo aggressive chemotherapy and lose his right upper arm bone. An avid golfer, he decided to have his entire shoulder socket removed and restored with a customized “reverse shoulder” replacement. It gave him complete range of motion, and within a year, he was golfing again.
The team at the OSUCCC – James was among the pioneers in using the implants for bone cancer patients about five years earlier, Dr. Mayerson says.
Previous reconstruction options for these patients had limited range of motion at the shoulder level. The newer replacements have been a game changer for many, Dr. Mayerson says, including a bus mechanic who was able to resume work following his implant.
Shultz remembers the first day he visited the OSUCCC – James.
“They were really positive. I distinctly remember Dr. Mayerson saying, ‘We want you to live a long life, we’re going to do everything we can for you.’ And I left there with a lot of hope,” Shultz says.
Shultz, who has been cancer-free since his December 2019 surgery, knows his disease is rare and is grateful that he lived so close to a place with such high-level sarcoma specialists.
“I have absolutely zero real limitations on how I live my life,” Shultz says. “I just think it’s amazing all the things that he does, and what he does for his patients.”
Finding new ways to improve sarcoma patient outcomes
Dr. Mayerson’s commitment has brought a number of other innovations to the OSUCCC – James.
Luke Skywalker limbs
Take, for example, what Dr. Mayerson calls the “Luke Skywalker effect” — referring to the prosthetic hand controlled by the “Star Wars” character.
Patients can control snap-on artificial limbs, and have less pain, through the use of techniques called osseointegration and targeted muscle reinnervation (TMR).
- Through the first technique, a surgeon implants a metal bar into existing bone. This serves as a point for external artificial limbs to attach and causes less discomfort than standard prosthetics.
- TMR involves sewing a severed nerve into a working nerve branch to another muscle, thereby preventing overstimulation of the nerve. This decreases post-procedural pain. When a special prosthetic can be directly connected to the TMR site, it leads to more natural movement and less chronic pain.
While these techniques, used in combination, are now only readily available in the military, experts at Ohio State offer both procedures individually and are working to find a cost-effective way to combine them for civilian patients who lose limbs to cancer.
Ankle-to-knee joints
 Surgeons at Ohio State have performed more than 15 rotationplasty surgeries to address tumors on or near the knee. During these procedures, the patient’s ankle is used as a new knee joint, with the foot reversed to serve as a shin bone where a below-the-knee artificial limb can attach.
Surgeons at Ohio State have performed more than 15 rotationplasty surgeries to address tumors on or near the knee. During these procedures, the patient’s ankle is used as a new knee joint, with the foot reversed to serve as a shin bone where a below-the-knee artificial limb can attach.
Because the procedure retains a joint, the patient uses less energy on walking and can be considerably more active than if an above-the-knee prosthesis was required, says Dr. Mayerson, a professor of Orthopaedics at The Ohio State University College of Medicine.
The procedure also allows the patient to run, twist and turn, functions that would be severely limited with standard artificial prosthetic limbs.
Surgery assistants
Dr. Mayerson was involved in developing “cutting guides” that can shorten the length of surgeries.
Imaging and 3D printing are used to create the guides, which help surgeons make precise cuts to remove tumors and surrounding bone. This could eliminate the need for the standard, and more time-consuming trial-and-error method done by hand.
The guides are made based on 3D models of a patient’s anatomy and are then pinned onto real bone during surgery, allowing the surgeon to clearly see where cuts need to be made.
The guides also are used to create made-to-size replacement bones that allow for an improved fit and hopefully improved longevity and function.

Cancer detectors
Dogs suffer from sarcomas at higher rates than humans, and a type of tumor detector for soft tissue cancer came out of a collaboration between the OSUCCC – James and The Ohio State University College of Veterinary Medicine.
Called optical coherence tomography, the goal is to take the machine into operating rooms at the OSUCCC – James, where surgeons can use it to scan tissue removed from a patient. Special lighting indicates the difference between healthy and cancerous areas, letting surgeons know immediately whether more tissue needs to be removed.
Raising a voice
 Dr. Mayerson’s tendency to push boundaries stretches beyond the operating room. With sarcoma being so rare, research dollars are hard to come by. So, he decided to find a way to generate a few.
Dr. Mayerson’s tendency to push boundaries stretches beyond the operating room. With sarcoma being so rare, research dollars are hard to come by. So, he decided to find a way to generate a few.
In 2010, he founded the Steps for Sarcoma 1-mile walk fundraiser, which has raised nearly $2 million for over 25 research projects.
In 2023, Dr. Mayerson’s efforts became personal. His mother died of a soft tissue sarcoma in her torso. She was treated at the OSUCCC – James, but the cancer had been found too late.
“It’s certainly motivated me even more to try to find a way to help people,” Dr. Mayerson says.
Funds from the walk have gone to researchers across various sites, including at the OSUCCC – James, the Ohio State College of Veterinary Medicine and Nationwide Children’s Hospital. And they’ve been used to explore groundbreaking topics, such as artificial intelligence, digital pathology and image analysis.
“The way he set it up is not to keep those funds in one place or for narrow, niche interests,” says Dr. Liebner, an associate professor of Internal Medicine at the Ohio State College of Medicine.
“The spirit that he’s trying to cultivate is that we all rise together. When patients do better, the program does better, everybody wins,” says Dr. Liebner.
It’s all an interesting twist for the kid from Lima in northwest Ohio who didn’t even really want to do this. He played sports and dreamed of becoming a sports medicine doctor. Then, in his fourth year of medical school at Johns Hopkins University in Baltimore he “got stuck” working in orthopedic oncology.
The first day, he was involved in a surgery to remove a bone tumor and insert a metal knee replacement. He was immediately hooked.
“I said, ‘Wow, this is really cool. I get to do orthopedics and save people’s lives at the same time. I want to do that,’” Dr. Mayerson says. “I sort of fell in love with orthopedic oncology that day.”

The experts at The James are pioneering new treatments and research for the more than 80 types of sarcomas
Trust your care to The James.
Learn more
Support Steps for Sarcoma
You can help raise critical funding for cancer research.
Give today