3D blueprint for surgeons improves head and neck cancer treatment at Ohio State
A futuristic lab is printing 3D models of patient anatomy and tumors to advance cancer treatment.
In the faces of his patients, Kyle VanKoevering, MD, sees the success of his work as a head and neck cancer specialist at The Ohio State University Comprehensive Cancer Center – Arthur G. James Cancer Hospital and Richard J. Solove Research Institute (OSUCCC – James).
“The most rewarding part of being an otolaryngologist for me is seeing a smile or satisfaction on a patient’s face when their quality of life is improved because of something we were able to help them with,” says Dr. VanKoevering, an associate professor in the Department of Otolaryngology – Head and Neck Surgery at The Ohio State University College of Medicine who focuses on treating patients with cancers of the skull base and nasal cavity.
Procedures to remove tumors from the highly complex anatomy of these regions can be difficult and challenging for surgeons, who sometimes encounter structural roadblocks to their intricate work.
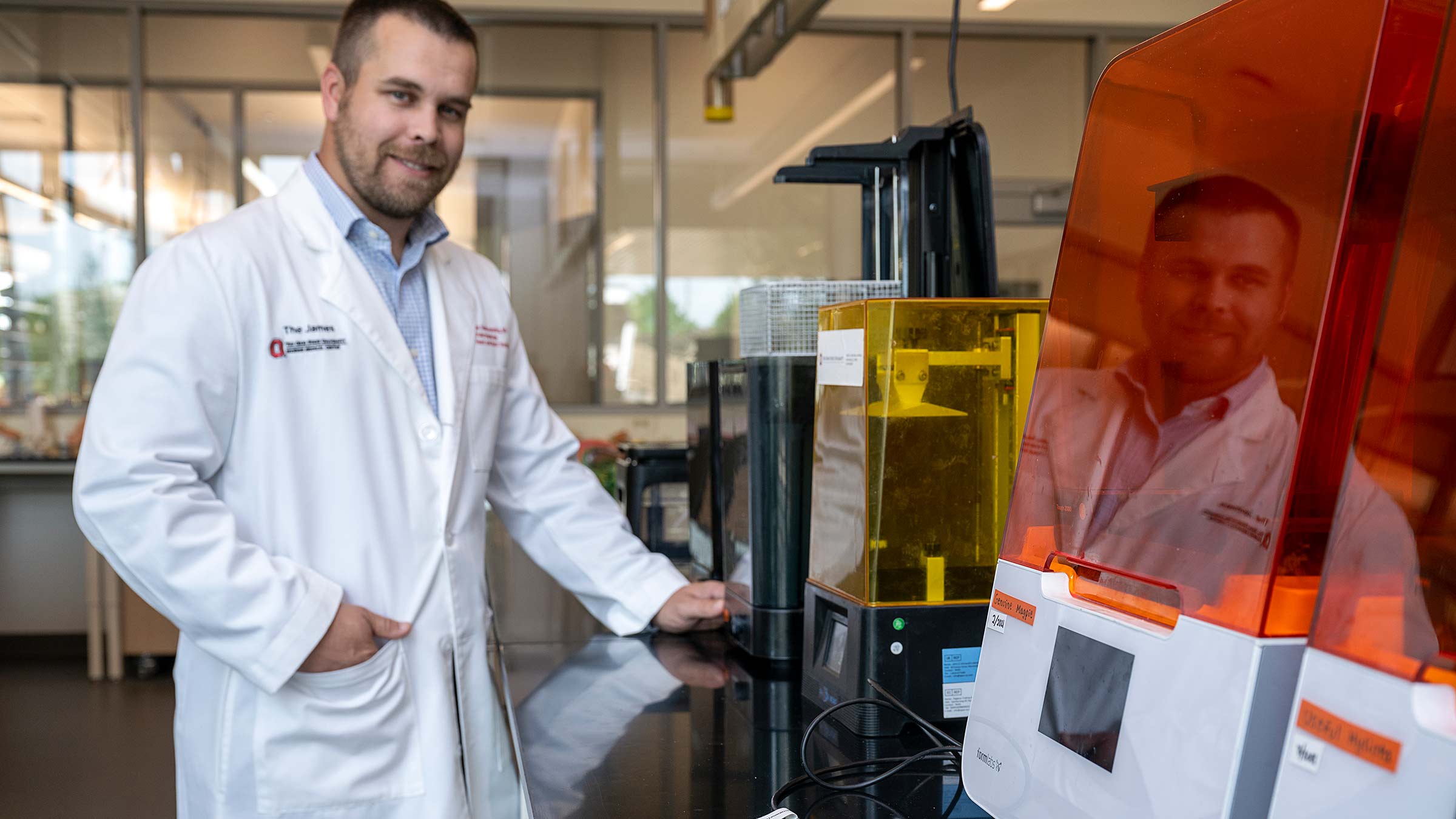
To help overcome these barriers, Dr. VanKoevering started and leads the Medical Modeling, Materials and Manufacturing (M4) Lab within the Ohio State College of Engineering’s Center for Design and Manufacturing Excellence (CDME). The M4 Lab is devoted to innovative 3D printing of patient-tailored anatomic models that surgeons can use in the operating room (OR) as guides for removing tumors and reconstructing bony anatomy with bone transplanted from elsewhere in the body.
“Once we’ve removed a tumor, we try to rebuild the facial structure in a way that the patient can still chew, talk and function in daily life,” Dr. VanKoevering says. “We used to have to eyeball it, but the M4 Lab has changed that.”
Dr. VanKoevering says 3D models printed to precisely match a patient’s anatomy are also invaluable for explaining, preparing or practicing for a surgical procedure before their use in the OR. “And these models are great teaching tools for our medical residents,” he adds.
Besides 3D modeling, the M4 Lab also supports the lifesaving efforts of medical professionals and other faculty via bioengineering (applying engineering principles to biology and biomedical technology) and medical-device development.
The lab brings together an interdisciplinary team of experts from the Department of Otolaryngology – Head and Neck Surgery, the CDME and Ohio State’s Institute for Materials Research who work collaboratively on these efforts.
The lab also receives internal funding support from the Center for Cancer Engineering – Curing Cancer through Research, Engineering and Sciences (CCE-CURES) program at the OSUCCC – James.
How 3D printed models are used in cancer surgery
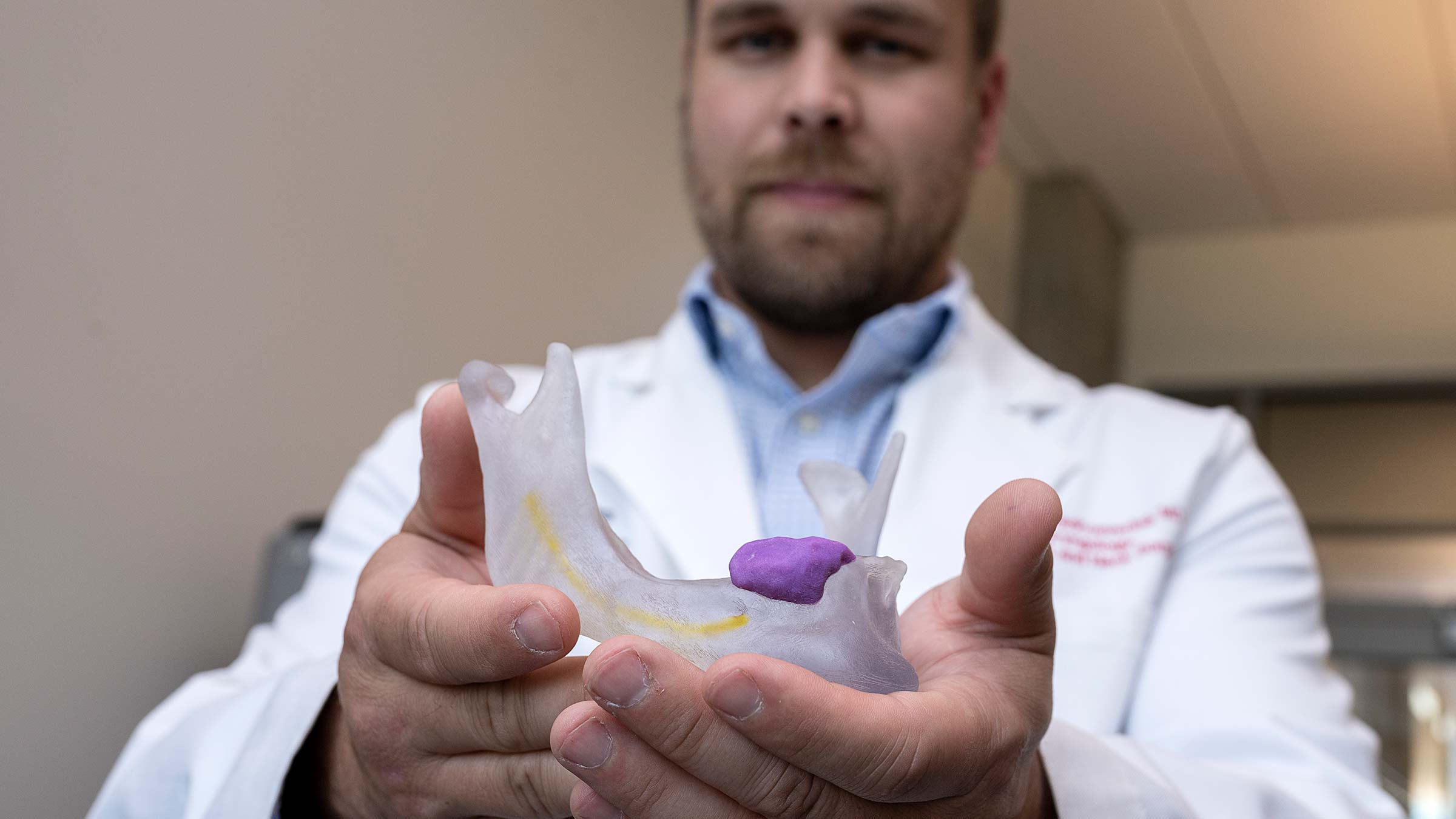
A sophisticated array of 3D printers allows for numerous fabrication methods and manufacturing capabilities inside the M4 Lab. In the past two years, biomedical engineering and clinical experts in the lab have assisted with nearly 200 surgical cases, starting with one in which they used a CT scan to create a replica of a patient’s mandible (lower jawbone) to facilitate reconstruction of the jaw after removing a segment of bone.
Many more cases have followed or are in the works.
“Basically, if we have a case coming up that involves complex reconstruction or a difficult tumor, our team takes the patient’s two-dimensional CT scans and MRIs and builds them into an exact 3D model of the anatomy of interest — the tumor, bone or whatever we’re looking for — and then we make a high-resolution medical-grade print of that, sterilize it and use it in the operating room,” Dr. VanKoevering explains.
“Often in these cases, one surgeon is removing a piece of bone and another surgeon is rebuilding the patient’s anatomy afterward with transplanted bone,” he adds. “The removing surgeon will take the 3D model and mark exactly where the cuts were made and where the bone is coming out, and then the reconstructive surgeon will bend plates to shape it to replicate the original anatomy.
“So when we put the patient back together and transplant new bone in there, we know as long as everything is lined up in the right locations, it’s all coming back together in the way that it should.”
Real-time 3D visualization enhances surgical reconstruction
In cases involving difficult tumors, Dr. VanKoevering says, “We’ll model the bone, the tumor and some of the arteries as well to precisely plan the entire surgical resection, thinking about things like how deep of the bony cut am I making, how deep of an angle do I need to take to get around the margin of the tumor, or how am I going to peel this off of a certain artery.”
Dr. VanKoevering says some of the projects underway in the M4 Lab include 3D modeling of:
- A patient’s maxilla (upper jawbone) in which a tumor is embedded in the maxillary sinus and is advancing toward the base of the skull
- A patient’s spinal tumor that’s intimately associated with the vertebral artery and will be difficult to remove
- A patient’s large pelvic tumor so the orthopedic oncologist can determine how best to resect (cut out) the tumor and reconstruct the bony component
“Our 3D models are sterilized and used intraoperatively in the OR for visual guidance,” Dr. VanKoevering says.
He points out that a surgeon typically can see only from one angle, which is sometimes hindered by blood, muscle and soft tissue.
“But you can hold a 3D model next to the patient, look it over and better understand the anatomy so you’ll know how best to proceed — things like, ‘I need to be moving from this angle,’ or ‘This is what structure I’m running into here’ or ‘I need to make a 4-centimeter cut there.’ That real-time feedback is really valuable.”

Leading research into expanded uses of 3D printing
As a member of the Translational Therapeutics Program at the OSUCCC – James, Dr. VanKoevering focuses his research on applications of 3D printing in medicine, clinical outcomes in skull-base malignancies, and developing solutions and devices for patients with tough-to-treat cancers.
He also leads clinical trials involving custom prosthetics that his team creates for patients via 3D design work, such as a specially tailored tube for laryngectomy patients that improves their voice box and enables them to speak.
“And we’re trying to start a first-of-its-kind prospective clinical trial that will look at modeling vs. no modeling and will prove for insurance purposes that custom modeling really does play out and have value in clinical outcomes,” Dr. VanKoevering says, noting that a private company is working with them to sponsor that trial.
A promising future for head and neck cancer treatment

He’s excited about possible future applications of 3D modeling at Ohio State as the technology evolves.
“I think we’re building one of the nation’s bigger enterprises around it, and that’s our goal. We have a lot of students, researchers and clinicians who are in this large ‘think machine’ that’s looking at patient outcomes, next steps, and material concepts and design features,” Dr. VanKoevering says, noting that they also have partnered with industry representatives to collaborate in these endeavors.
“One of the things I’m really impressed with at Ohio State is the collaborative culture and community among the various disciplines in head and neck cancer treatment — working closely together and bouncing ideas off each other so we can build the best treatment plan possible for our patients,” he says. “With so many partners, it’s fun to be a part of this space.”

Your support fuels our vision to create a cancer-free world
Your support of cancer care and pioneering research at Ohio State can make a difference in the lives of today’s patients while supporting our work to improve treatment and reduce cases tomorrow.
Ways to Give