Reinventing the way gastrointestinal diseases are diagnosed and treated
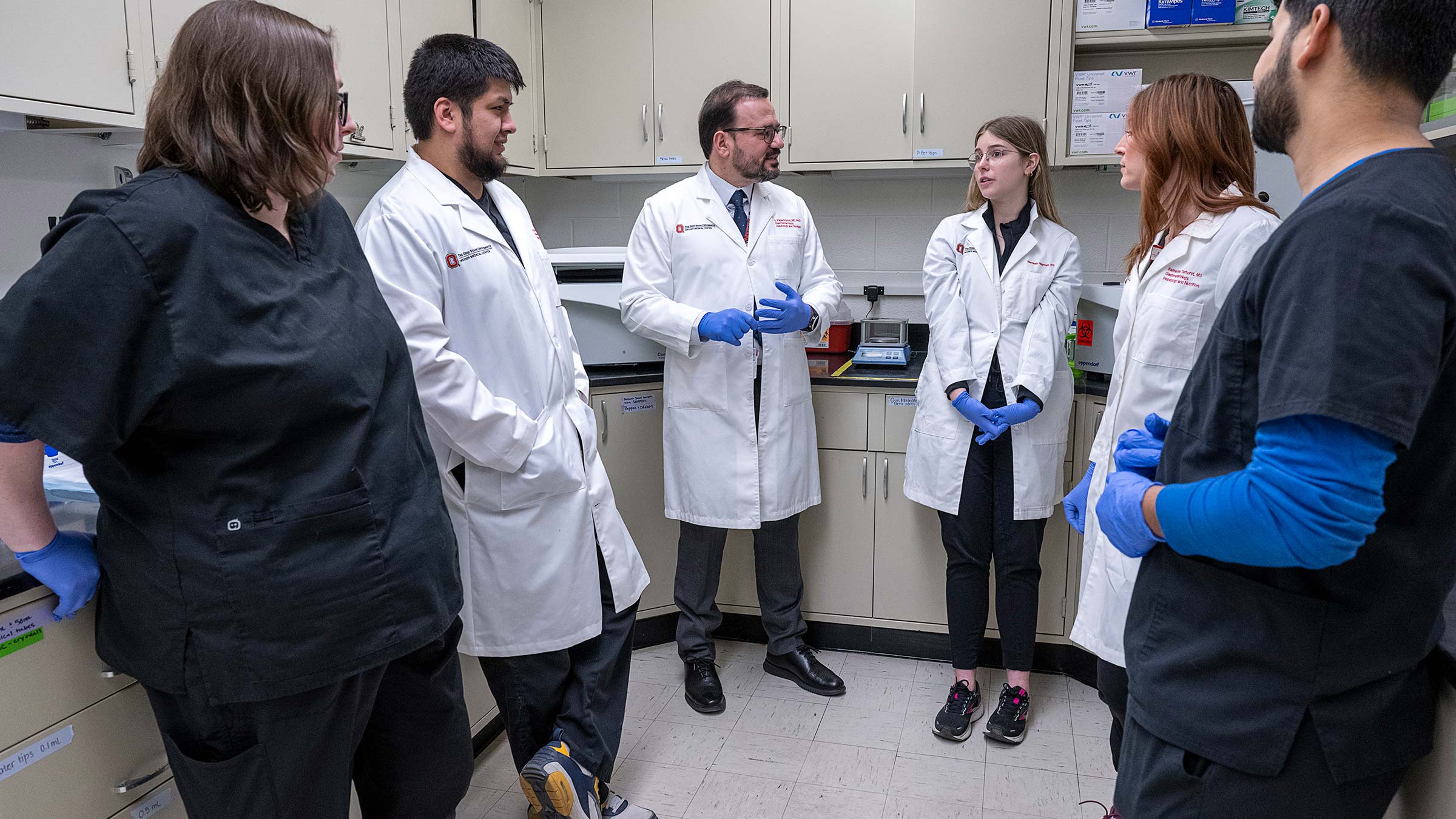
In the endoscopy room and the research laboratory, Dr. Georgios Papachristou is expanding the scope of care for gastroenterology patients.
Every year in the United States, 300,000 people are admitted to the emergency department in unbearable pain from acute pancreatitis, a serious condition that involves sudden inflammation of the pancreas.
Acute pancreatitis has long been considered a “black box” for physicians — a seemingly impenetrable mystery that defies accurate prediction. It is more common in middle-aged and elderly people, but it can strike the young as well. It is often related to gallstones and alcohol use, but lifestyle is only one piece of the puzzle.
There is no treatment or cure for acute pancreatitis — only measures to make patients more comfortable until their symptoms resolve. While 80% of patients will recover on their own, the other 20% run the risk of organ failure or death. But, until recently, it was anyone’s guess who would fall into this unlucky 20%.
A skilled researcher and gastroenterologist at The Ohio State University Wexner Medical Center, Georgios Papachristou, MD, PhD, is exploring the “black boxes” of gastroenterology to better understand who’s at highest risk for developing conditions like acute pancreatitis, and how to improve their outcomes through advanced procedures and therapeutic drugs.
A ‘single procedure’ to diagnose and treat gastrointestinal conditions
A native of Patras, Greece, Dr. Papachristou had a natural bent toward science, combined with the presence of strong role models in the field. Going to medical school was an easy decision.
But unlike most medical students, he knew he wanted to forge a dual career path in research and clinical medicine. “I had several fantastic instructors who inspired me with the way they integrated research into their practices for the benefit of patients,” he says.
After medical school, he moved to the United States to complete an internal medicine residency at Albany Medical College before embarking on a fellowship in gastroenterology at the University of Pittsburgh.
“I was always interested in the physiology of disease at an intellectual level, but I also wanted to use my hands by undertaking complex procedures,” Dr. Papachristou says. “Gastroenterology combines the best of both worlds.”
As a fellow, Dr. Papachristou began to build expertise in two advanced procedures. The first, endoscopic retrograde cholangiopancreatography (ERCP), is geared toward treating problems in the bile and pancreatic ducts. During an ERCP procedure, Dr. Papachristou guides a thin, flexible tube called an endoscope through the esophagus and stomach to reach the upper part of the small intestine. The endoscope is fitted with LED lights and a tiny video camera, affording a better view of what is going wrong.
The second, endoscopic ultrasound, is a newer technology that places an ultrasound probe at the tip of an endoscope to examine the inside of the digestive tract and diagnose everything from pancreatic and colon cancer to inflammatory conditions such as pancreatitis.
During his fellowship years, gastroenterologists used these procedures only to diagnose problems — not treat them.
“We were searching for an opportunity to help patients more directly,” Dr. Papachristou says. “That is where therapeutic endoscopy comes in.”
Therapeutic endoscopy, which he went on to study at Mayo Clinic, requires tremendous technical skill to accomplish a medical feat: a single procedure to diagnose and treat gastrointestinal conditions. Now, immediately after Dr. Papachristou identifies a problem while performing ERCP or endoscopic ultrasound, he inserts small instruments through the endoscope to confront it, whether that means breaking up and removing stones, placing stents to open ducts, or removing tumors or tissues to biopsy.
New tools and techniques reinvent care of patients with gastrointestinal diseases
After 13 years of helping lead a robust program at the University of Pittsburgh, Dr. Papachristou arrived in Columbus in 2019 to continue this success at the Ohio State Wexner Medical Center.
“There was already such a momentum and investment in resources at Ohio State,” says Dr. Papachristou, who currently serves as the division director for Gastroenterology, Hepatology and Nutrition and holds the Dr. Floyd M. Beman Chair in Gastroenterology at the Ohio State College of Medicine. “We have all the right elements in place to make our division one of the best in the country.”
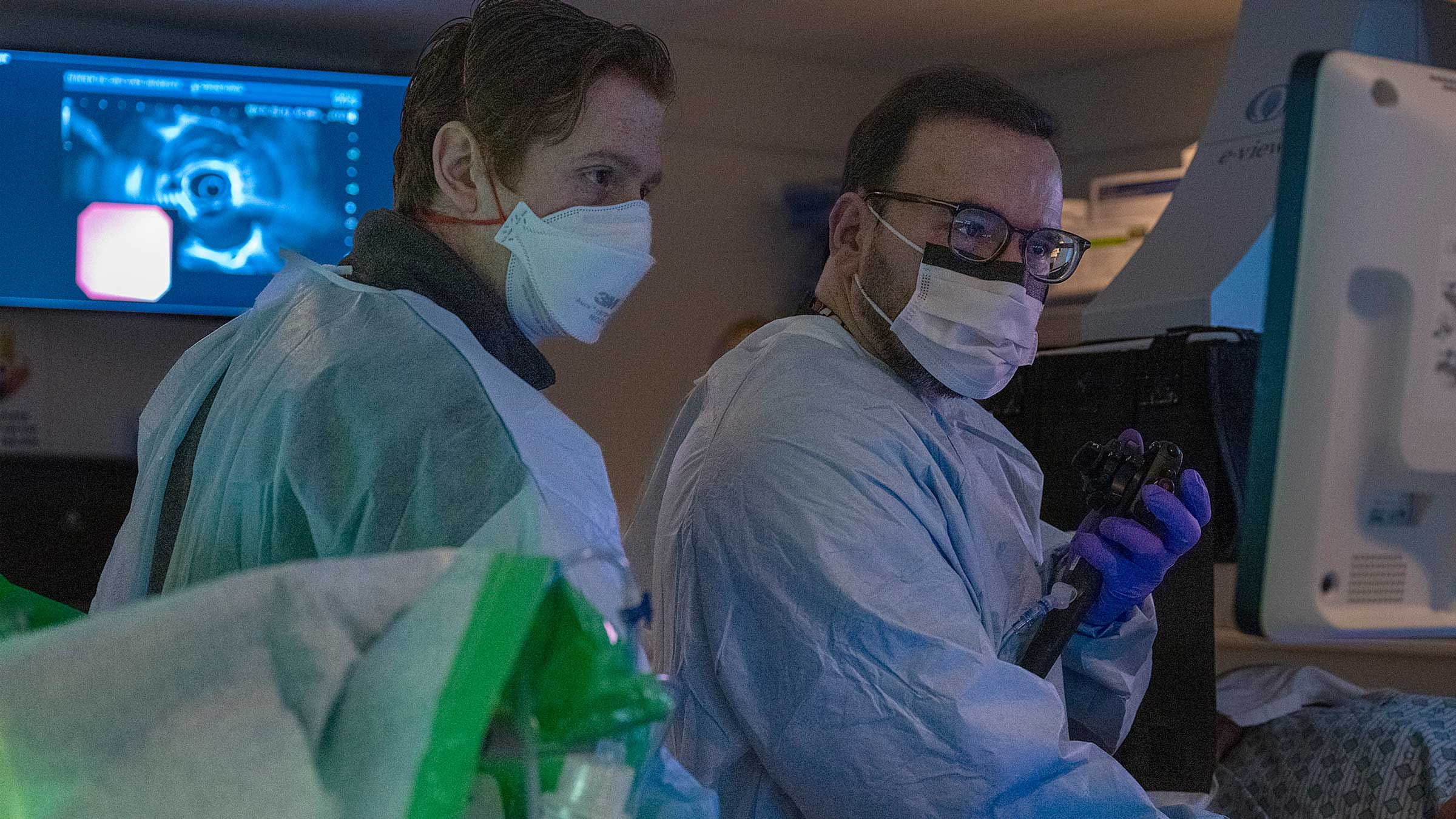
Dr. Papachristou pushed to recruit physicians skilled in therapeutic endoscopy to meet the growing demand for minimally invasive procedures. Eight of the 40 members of the division he leads spend their days performing ERCP procedures and endoscopic ultrasounds.
Thanks to recent advances in therapeutic endoscopy, procedures that once required several days of hospitalization are now so minimally invasive that they are considered outpatient. “We are constantly trying to reinvent ourselves with new tools and techniques,” Dr. Papachristou says.
In patients with narrowing of the small intestine, for example, Dr. Papachristou and his colleagues would previously have to request a surgical bypass. Now, they can place a stent that connects the stomach to a free loop of the small intestine and achieve the same outcome. Likewise, draining large fluid collections in patients with necrotizing pancreatitis (dead pancreatic tissue) used to take hours, because the endoscopic process involved surgical tools designed for other purposes. Dr. Papachristou was part of a team at Ohio State that implemented the use of a new technique with the capacity to drain fluid within a few minutes with superior results.
Luis Lara, MD, the medical director of endoscopy at the Ohio State Wexner Medical Center, credits Dr. Papachristou with “putting the right people in the right places with the right technology.” As a result, Ohio State’s gastrointestinal program is evolving from a reputable clinical program into one of the country’s premier programs. “There are only a few programs in the United States that are able to do what we do here,” Dr. Lara says. “Under Dr. Papachristou’s leadership, ours is quickly becoming a standout.”
Accumulating wins in acute pancreatitis research
Dr. Papachristou is equally committed to advancing patient health in the research laboratory.
As a fellow at the University of Pittsburgh, Dr. Papachristou studied under a physician who ran a research program focused on acute pancreatitis. He quickly became intrigued by this poorly understood disease. Even the world’s leading gastrointestinal experts were at a loss for how to treat acute pancreatitis, which can lead to organ failure, necrosis of the pancreas or even death in the 20% of patients who develop more severe cases.
“The problem is that we had no accurate way to predict which cases would fall into this 20% and which would resolve without further intervention,” Dr. Papachristou says.
“My mentor urged me to forget what I had learned and try to rewrite our collective understanding of the disease.”
Over the past two decades, he has taken his mentor’s words to heart.
In the field of acute pancreatitis, Dr. Papachristou is best known for studies like Pancreatitis-associated Risk of Organ Failure (PROOF), which identified five proteins that serve as markers of inflammation. With 90% sensitivity, these biomarkers have the potential to accurately predict which patients will develop a more severe form of acute pancreatitis.
Peter Lee, MB BCh, who conducts research in acute pancreatitis alongside Dr. Papachristou, says he is a “true pioneer in his field.” Before he came on the scene, the largest acute pancreatitis study that existed had only recruited several hundred patients. Then, Dr. Papachristou fostered collaboration on an international scale to recruit upwards of 1,500 patients for the landmark Acute Pancreatitis Patient Registry to Examine Novel Therapies in Clinical Experiences (APPRENTICE) study. “Dr. Papachristou has a rare ability to bring people together to drive a project like this forward,” Dr. Lee says.

Turning research into tools to treat acute pancreatitis and improve patient care
Now, Dr. Papachristou, Dr. Lee and their colleagues are embarking on a project to formally validate the results of the study before implementing it in clinical practice. If validated, it will offer the first-ever tool for separating mild from severe cases of acute pancreatitis, improving quality, cost and efficiency of patient care.
Novel biomarkers will also lay the groundwork for the development of the first drugs specific to acute pancreatitis.
As they work on the validation study, the members of the Papachristou Lab are also immersed in two other studies related to acute pancreatitis. The first, a multicenter study funded by the National Institutes of Health (NIH), is focused on uncovering the prevalence and consequences of diabetes after an attack of acute pancreatitis. For unknown reasons, some of the patients who recover on their own within several days and return home will develop diabetes. The second study, another NIH-funded multicenter study, is targeted at preventing the development of pancreatitis following an ERCP procedure.
These studies, among others, have built Dr. Papachristou’s reputation as a “top 10 international expert in acute pancreatitis research and treatment,” says Philip Hart, MD, the director of clinical research for the Division of Gastroenterology, Hepatology and Nutrition.
Dr. Papachristou is also eager to build on the model of pancreas research to generate impactful research in areas like inflammatory bowel disease, hepatology and liver transplant, and neurogastroenterology. From identifying therapeutic treatment options for the millions who suffer from irritable bowel syndrome (IBS) to improving postsurgical immune response in the Ohio State Wexner Medical Center’s busy liver transplant program, there’s no shortage of questions to explore.
“As a leader, my goal is to train and equip the next generation of gastroenterologists to meet unmet needs in innovative ways,” Dr. Papachristou says. “As clinicians and researchers, we have an opportunity to reach the next level of patient care.”

When you give to The Ohio State University Wexner Medical Center, you’re helping improve lives
We’re committed to making advancements in research, education and patient care that will have an impact throughout Ohio and the world.
Ways to Give




