If you’re at increased risk for heart disease, a coronary artery calcium scan could tell you if you need more testing and prompt you to make healthy lifestyle changes.
Changes aren’t easy, but your provider can help you find the support you need.
Every 40 seconds, someone in the United States has a heart attack.
Eating choices, physical activity and medications, when used together, can help lower your risk of a heart attack.
What are coronary artery calcium scans?
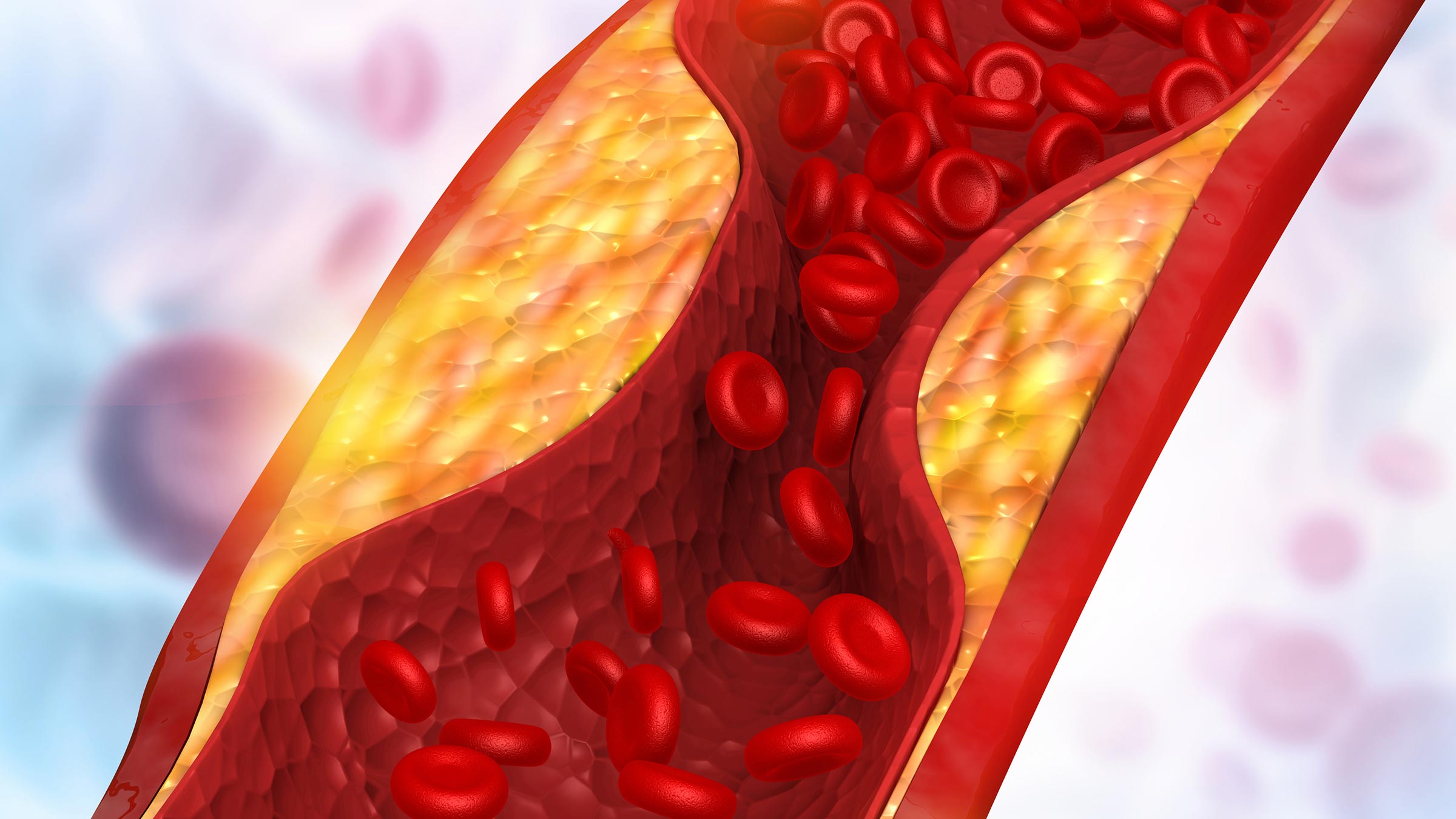
Coronary artery calcium scans are low-dose computed tomography (CT) scans of the chest to detect calcified material, or plaque, in and around the coronary arteries.
Coronary artery calcium scans require no preparation and are painless.
If the plaque buildup is detected earlier in life than is typical, or if there’s more plaque buildup than is expected, then this can indicate an increased risk for cardiovascular disease, including heart attack and stroke.
Most heart attacks and strokes are caused by disruptions or clots in the plaque located in the arteries of the heart or brain, leading to damage from the decreased blood flow.
Limitations of calcium scans
A coronary artery calcium scan won’t tell you how much an artery is blocked. Rather, it estimates the overall burden of plaque-formation that your coronaries have experienced leading up to this point in life.
We have other tests to collect more information:
Stress tests demonstrate how vigorously the heart functions and receives the extra blood flow necessary to allow physical exertion (such as walking/running on an incline treadmill).
CT coronary angiograms are heart scans that use IV contrast to get a more detailed picture of the coronary arteries.
Invasive coronary angiograms are done as part of a heart catheterization, often known as a “heart cath,” to find blockages in the coronary arteries. Often, certain blockages can be treated in the same procedure with balloon and/or stenting techniques.
Who should get a calcium scan?
The coronary artery calcium scan is not for everyone. It can be most useful in those who are at intermediate risk of heart disease.
For example, those who have a significant chance (e.g., a 10-20% chance) of experiencing a heart disease event in the next decade but who aren’t yet taking certain medications such as statins or other cholesterol-lowering drugs, aspirin, blood pressure lowering medications or anti-diabetes agents.
If you have a family history of premature heart disease, you’re likely a good candidate for the test, usually starting at age 40 or so.
How are calcium scans scored?
The results of a coronary artery calcium scan include a summary of how much calcified material is associated with each of the major coronary arteries and their branches — the left main, left anterior descending, circumflex and right coronary arteries.
There’s also a total score reported, which is usually the most helpful metric to determine how the amount of calcified plaque compares to most people of that age.
We often use a reference tool based on data from the Multi-Ethnic Study of Atherosclerosis (MESA) paired with your calcium scan score to estimate whether you have below- or above-average calcification for your age, gender and racial/ethnic category.
If you’re younger to middle-aged, you should have no evidence of calcified plaque.
Even a small amount of calcified plaque detected earlier in life could mean early or accelerated atherosclerosis. Your doctor can use additional testing to see if you need preventive therapies to reduce your chance of having a heart attack or if you need a heart catheterization procedure.
What to know if you have high results
If you have significant plaque buildup, don’t panic. Be grateful that you’ve caught your risk factors before a heart attack happens.
Heart disease is preventable to a very large degree, so I try to motivate my patients at higher risk with careful counseling about what they’re eating and how much physical activity they’re getting. We also go over medications that can work to lower their risk.
Not all risk factors are modifiable — you can’t change your age or family history — but many others can be improved greatly by a combination of medications and lifestyle changes.
You can be at increased risk if you have high blood pressure, diabetes, use tobacco or are obese.
Ask your doctor to check your cholesterol if that hasn’t been done in the last year, or if you’ve not reassessed it after changing your diet.
Blood tests could include a standard lipid profile (cholesterol test) and, in some cases, also include additional tests such as the lipoprotein(a), apolipoprotein B, or LDL particle numbers, which can help your doctor determine if you have a higher cholesterol-related heart disease risk than a standard lipid profile might suggest.
If a patient has previously had high scores and is having potential symptoms of heart disease, such as increased shortness of breath or chest discomfort with exertion, then I will recommend additional testing.

Your heart is in the right place
Learn more about advances in care and treatment for patients at The Ohio State University Heart and Vascular Center.
Expert care starts here




