ECMO providing new opportunities for critically ill patients to recover
Ohio State is one of the few medical centers capable of delivering this lifesaving treatment.
When Mike Kaster contracted COVID-19 in 2021, there was little reason to think that the disease would ravage him as badly as it did.
Kaster, of Carmel, Indiana, was 59 at the time but very active — working out four to five times a week while training for a half-marathon. But once he contracted the virus, his health deteriorated rapidly.
By early August, his situation had become dire. He was on a ventilator at a hospital in Indianapolis and needed a double lung transplant, as well as a cardiac bypass for a blockage.
“For my wife, Joan, and all of us, it was a big surprise,” Mike recalls. “They told her, ‘We don’t have a lot of hope at the moment. Call your family, bring them in to see him.’”
The Ohio State University Wexner Medical Center took over his care, and he woke up there about a month later, having received the double lung transplant and the bypass.
One critical component of his recovery was extracorporeal membrane oxygenation (ECMO) treatment, a lifesaving procedure that can help supply patients awaiting transplant with more time to wait for an organ to become available.
Right: Kaster has since recovered and is actively exercising again.
How ECMO works
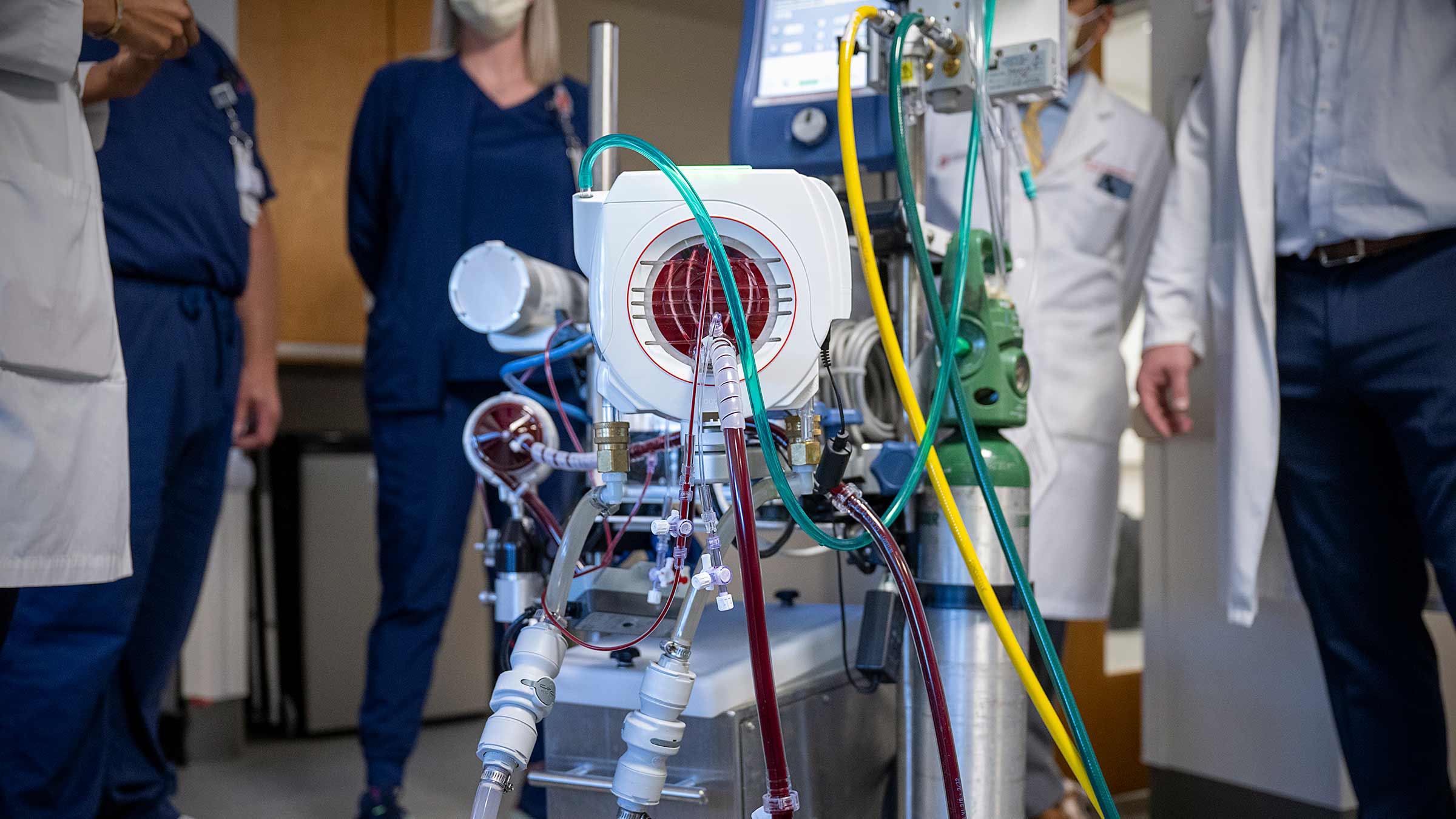
ECMO supports patients in cardiac or respiratory failure by moving the functions normally performed by the heart or lungs to a complex heart-lung bypass machine attached to the body. This allows the heart or lungs to rest, often while a patient awaits a transplant. Management of ECMO patients requires a team of highly skilled medical professionals and the resources of large, academic medical centers like Ohio State. Patients on ECMO require around-the-clock care from a broad array of experts.
ECMO is the most advanced form of life support available. Blood is drawn out of the body and diverted to a device that oxygenates the blood, removes carbon dioxide and then returns the blood back to the patient. It does the work of the lungs in patients with severe respiratory failure when a ventilator is not providing adequate support, or when there is a possibility of lung injury.
“ECMO is a team sport,” says Veena Satyapriya, MD, a critical care anesthesiologist in the cardiovascular intensive care unit who serves as medical director of the ECMO program at the Ohio State Wexner Medical Center. “It requires a collaborative team of highly skilled physicians, perfusionists, nurses and respiratory therapists to ensure the best possible outcomes for our patients, whether we are looking to bridge them with ECMO to lung recovery or to lung transplant if the lungs do not recover, as was the case with Mr. Kaster.”

New transportation initiative was key
In Mike’s case, the Ohio State Wexner Medical Center was able to take him as a patient because of a partnership with medical transport service MedFlight to bring ECMO patients to Columbus for treatment.
Because the program, known as the ECMO Retrieval Program, involves Ohio State medical experts caring for the patient in a mobile intensive care unit during transportation, it allows for a broader range of patients to be considered. Before the program was implemented in 2022, smaller hospitals often could not get patients to Ohio State for care because they did not have sufficient staffing resources to do so.
Mike was the second patient to be transported under the program.
“We provide specialized care for patients with cardiac and respiratory failure requiring ECMO, and proudly serve as partners to regional medical centers who may not have the resources and expertise to care for patients this sick,” Dr. Satyapriya says. “This program is increasing access and reducing disparities in care to the sickest patients in the region.”
Typically, a patient is on ECMO for about two weeks. But Mike remained on ECMO until he received his double lung transplant and a coronary bypass at the Ohio State Wexner Medical Center, 101 days after he was first hospitalized in Indiana. After receiving the transplant and bypass, Mike recovered quickly and has returned to running.
“I have angels looking over me,” he says. “ECMO is what kept me alive to get the transplant.”

A team-based approach
The process to administer ECMO to a patient is a complex one involving a wide array of medical professionals.
“It’s a huge team effort. These patients are very resource-intensive, very sick. There is so much that goes into it,” says Asvin Ganapathi, MD, cardiac surgeon and surgical director of the ECMO program.
That team includes the patient’s surgeon, anesthesiologists, perfusionists (medical experts who specialize in oxygenating blood outside the body), nurses and operating room staff, among others. Patients undergoing ECMO require 24/7 monitoring in a critical care unit. When deciding whether to put a patient on ECMO, the group is mindful that it’s a temporary treatment designed to get the patient to the next step.
“To me, what makes our program a differentiator is we have this amazing, robust multidisciplinary team,” Dr. Satyapriya says.
“The work can be physically and emotionally demanding, and while mortality is high in this line of work, we have seen patients like Mr. Kaster make it out of the hospital and back home to their families, their lives. That keeps us going.”

The pandemic put ECMO at the forefront of treatment
The Ohio State Wexner Medical Center treated more than 100 ECMO patients per year in the five years preceding the COVID-19 pandemic, but that number grew to 175 in 2021.
Additionally, the pandemic brought additional focus on the role ECMO can play in helping patients with acute respiratory distress syndrome (ARDS). In many ARDS patients, ECMO can supply oxygen to the blood without the risks of lung injury that come with mechanical ventilation.
“We are offering something that only about 100 centers nationwide can offer — a potential lifesaving therapy, both in the form of ECMO and the therapy after,” says Dr. Ganapathi. “What differentiates Ohio State is our ability to take care of ECMO patients, then transition them to a long-term therapy.”

Your heart is in the right place
Learn more about advances in care and treatment for patients at The Ohio State University Heart and Vascular Center.
Expert care starts here