Nurse and patient’s support group improves options for pulmonary arterial hypertension patients

Debbie Kittel, BSN, RN, CCRN, calmly watched the scene unfold before her, waiting for her cue. It came when the 30-year-old patient, Tiffani Brown, started sobbing at the news her shortness of breath was caused by a rare, progressive heart and lung disorder called pulmonary arterial hypertension (PAH). The news stunned Brown, who came alone to her appointment with a cardiologist at The Ohio State University Wexner Medical Center. She’d assumed that she’d just be told to lower her stress and lose weight. Instead, she learned that she was in a life-and-death health crisis.
“You’re close to death because your heart is in severe heart failure,” Brown recalls being told in June 2020.
That’s when Kittel stepped forward, her empathy and training kicking in as pulmonary arterial hypertension nursing program manager at the Ohio State Wexner Medical Center’s Richard M. Ross Heart Hospital. She calmly and simply explained what pulmonary arterial hypertension is, opening and closing her hand to describe how the arteries in the lungs become narrow or blocked, slowing blood flow through the lungs. That causes the heart to become weak or fail as it works harder to pump blood through the lungs.
“I’d never heard of pulmonary arterial hypertension before. Debbie explained it all to me and has been there for me since day one,” Brown says. “Now we’ve joined together to start a support group to help others struggling with this.”
A nurse’s unwavering concern for her patient after pulmonary arterial hypertension diagnosis
Over the past two years, Brown has turned to Kittel whenever she needed help getting through hard times. Brown’s medical condition forced her to quit her job as a school bus driver and go on disability leave. Like many others during the pandemic, she isolated herself. Recognizing the depression setting in for her patient, Kittel was determined to get Brown out of the house and moving for both her physical and mental health. When she learned they lived near each other, Kittel hired Brown to walk her dogs.
“It was heartbreaking to watch such a young, lively and bubbly person stay in bed all day. During the pandemic, we saw a lot of patients who were really deconditioned because they were not going to pulmonary rehab. While walking the dogs and talking with Tiffani, I realized how much a pulmonary hypertension support group was needed in our area,” Kittel says.

Brown felt the same way, especially after learning how dangerous a suggestion was that she’d gotten online from another PAH patient on how to swim by disconnecting her PAH pump. Brown later learned that every time she unplugged her pump to swim, she was stressing her heart and causing more damage. Anecdotes like this inspired Kittel to start a support group with a health care provider present to dispel misinformation.
“While my family has been amazing and supportive, I didn’t have anybody who understood my typical day and how I feel,” Brown says.
“Debbie had been wanting to start a support group for a long time and asked if I’d be interested in starting one and I said ‘Yes, please!’” says Brown.
Fellowship and experts are key part of pulmonary arterial hypertension support group
On a warm summer night, Kittel is arranging plates of low sodium vegetable pizza on a table in the Ohio State Richard M. Ross Heart Hospital when she hears her name being called. She bounds toward the door and pulls a PAH patient into a hug.
“If you’re here, I’m here,” the patient says, smiling and taking in the room where about a dozen others are gathered.
It’s the third meeting of the support group that Brown and Kittel started in March 2022. The two are wearing T-shirts they’re selling to raise awareness about pulmonary hypertension and help fund the group’s upcoming low sodium Thanksgiving meal. About 50 nurses from the Ohio State Wexner Medical Center have bought the shirts so far.
After a moment of silence for those who have died of pulmonary hypertension, Elie Homsy, MD, a pulmonologist at the Ohio State Wexner Medical Center, delves into an informative session about how to safely travel by airplane. “I don’t have pulmonary hypertension, but I learn a lot from you,” he says after answering questions from the group. Topics at this meeting and others have included home oxygen therapy, pulmonary rehab and exercise, working with PAH, current research studies and diuretic management as well as open discussion time for patients to share tips and build relationships with others dealing with PAH.
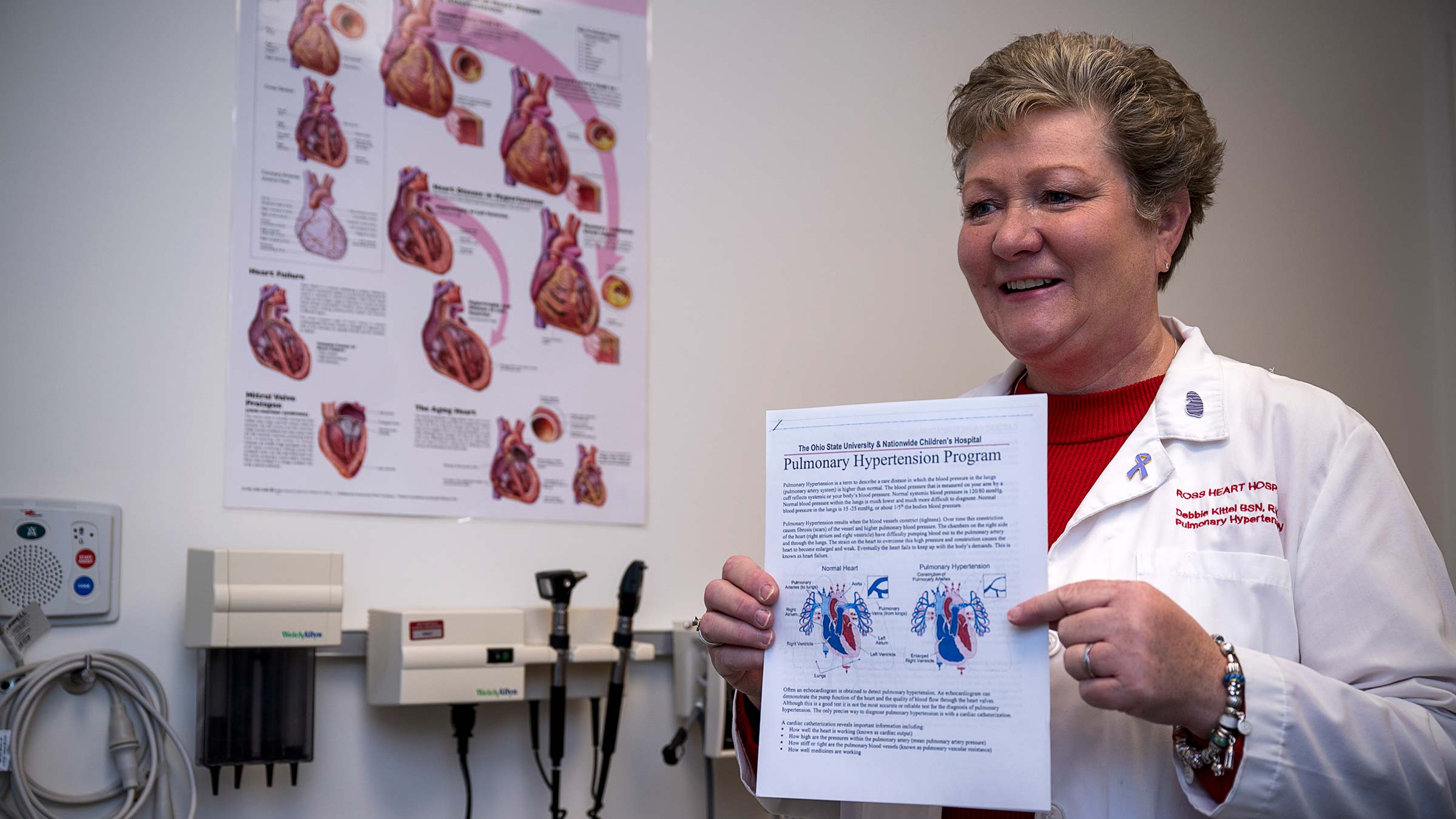
Having a physician, pharmacist, nurse or other expert answer questions during the meeting is critical. “That way, if someone says they saw some advice on social media, our expert can give the medical side of it,” Brown says.
Both Kittel and Brown are thrilled with how the support group has helped those living with PAH and the friendships being created.
“A young guy with pulmonary arterial hypertension came to the support group when we discussed mental health, and the next time I saw him, he was a different person. He’s thinking of going back to school and wants to be a social worker. It was great to see him grow and come out of his shell,” Kittel says.
Seeking solutions, improving life for PAH patients
Living with PAH can be challenging, and not only has Kittel been with Brown every step of the way, but she’s also come up with ideas to improve other patients’ lives. For some patients like Brown, they have a medical pump inserted under their skin in the fatty tissue, which is extremely painful for about a week. “Like a knife stabbing you in the stomach” is how Brown describes it, saying the prescription topical pain medication doesn’t do much to relieve the site pain.
Kittel has been working with industry representatives to help develop innovative ways to better deal with PAH pain. She’s also been talking with manufacturers about whether larger, waterproof dressings can be made so that Brown and others can safely swim without unplugging from their unit, which can cause serious health problems.
Proud of how her care has extended beyond the medical setting, Kittel shares how she played a role in Brown’s returning to school, where she’s now seeking certification in medical billing and coding. Kittel provided her with information about Opportunities for Ohioans with Disabilities, a state agency that has helped guide Brown in employment options. Kittel was familiar with the agency because it had helped her son, who is autistic.
Walking and talking with Brown has made Kittel realize she needs to take better care of herself, too. The self-described workaholic has started exercising, spending more time outdoors and taking time off for herself.
“Tiffani has made me more aware of my own mental health,” Kittel says. “She has given back to me as much as I have given to her.”
Interested in joining the Ohio State Pulmonary Arterial Hypertension support group? Email us here.

Your heart is in the right place
Learn more about advances in care and treatment for patients at The Ohio State University Heart and Vascular Center.
Expert care starts here