20 years of cardiovascular care advancements save more lives
Big leaps take heart and vascular care from science fiction to standard procedure at the Ohio State Richard M. Ross Heart Hospital.
When Ernest Mazzaferri Jr., MD, reflects on how heart and vascular care has changed in the past 20 years at The Ohio State University Wexner Medical Center Richard M. Ross Heart Hospital, he can’t help but evoke the memory of his father. “My dad was a physician and used to say he would give anything to see where medicine will be in 100 years,” says Dr. Mazzaferri.
Heart and vascular care is changing so rapidly now that it’s hard to imagine patient care in the next five years, let alone 100.
What seems like decades of advancement occurs every few years, making cardiovascular care feel more like science fiction than reality. “You can’t practice cardiology like you did even three years ago, or you’re out of date,” Dr. Mazzaferri says.
Five major advancements in cardiovascular care
Thanks to less invasive treatments, preventive medicine and better screening and treatment technology, more patients than ever are living longer, healthier lives.
Five major advancements in cardiovascular care illustrate how patient outcomes have improved in the two decades since the Ohio State Richard M. Ross Heart Hospital opened its doors in 2004.
1. Minimally invasive procedures add years to patients’ lives
Twenty years ago, elderly patients had limited options when it came to treating cardiovascular disease. Patients too frail to undergo open heart surgery would linger in the hospital before dying or entering hospice care.
Today, many patients in their 90s receive a minimally invasive, life-saving procedure in the catheter laboratory (cath lab). After a few days, they return home with a new lease on life.
That’s thanks to the transcatheter aortic valve replacement (TAVR) procedure, which is the most significant recent advancement to heart and vascular care, according to cardiothoracic surgeon Bryan Whitson, MD, PhD. TAVR is an alternative to open heart surgery in which doctors replace a narrowed aortic valve by guiding a catheter through an artery in the patient’s groin or armpit; the catheter is guided to the heart to deliver a new valve.
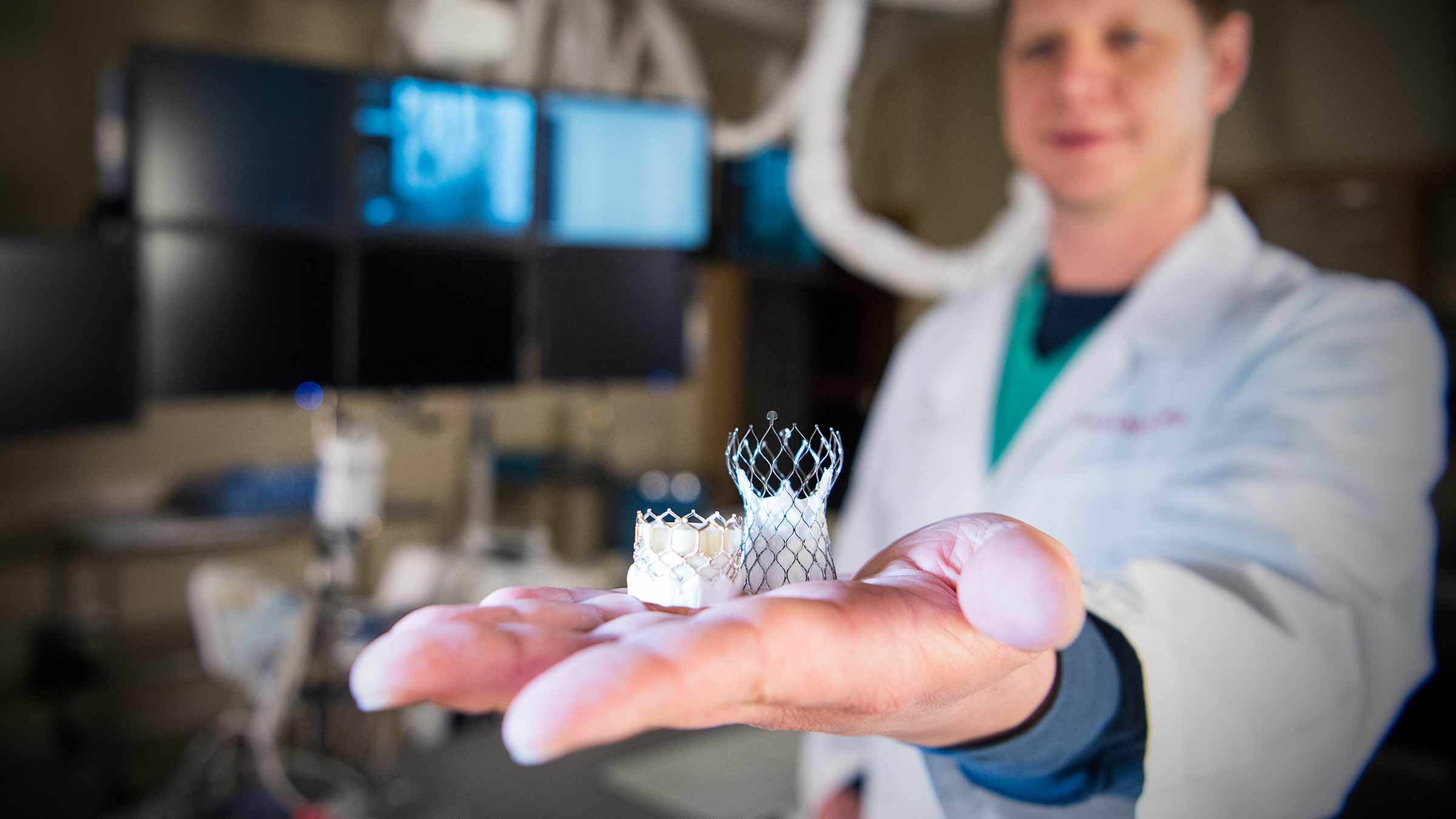
“Patients are recovering more quickly and going home because they don’t have big surgical incisions,” Dr. Whitson says.
One patient in her early 70s with a history of breast cancer needed her heart’s mitral valve replaced. She had previously undergone a mastectomy and breast reconstruction, making another surgery in the chest area complicated.
“We’re able to offer therapies today that would have been inconceivable back in 2004,” Dr. Whitson says.
In the past, her options would have been to live with the leaking valve or replace the valve by opening her sternum (breastbone). Instead, her doctors repaired the valve through a small keyhole incision in her armpit. She returned home after three days with minimal pain and was back to full function in four to six weeks.
One of Dr. Mazzaferri’s first TAVR patients was a 96-year-old woman. “Before TAVR, there’s nowhere on the planet where she would have had therapy options. She went on to live until she was 99, when she died of another cause,” he says.

As technology advances and gets smaller, more minimally invasive heart and vascular procedures become available every year.
In many cases of an aneurysm — a bulge in a blood vessel wall that can be deadly when it ruptures — patients can be treated through a catheter instead of a major operation.
“Back in the late ’90s and early 2000s, we heard this was happening and said there’s no way that’s ever going to work. Now it’s become a standard of care,” Dr. Mazzaferri says.
2. Rapid response to cardiovascular emergencies
One father in his late forties remains cemented in Dr. Whitson’s mind. The man started feeling sick at work and laid on his office couch. His partner found him unresponsive with no heartbeat and called 911.
Twenty years ago, first responders would have likely called the time of death once they arrived. Today, they were able to rush him to the hospital after shocking his heart with a mechanical chest compression device that pumped blood for him.

There, he was attached to a temporary heart and lung machine while doctors in the cath lab opened his blocked artery.
“He was technically dead while his heart wasn’t beating on its own. He’s having a normal life with his family instead of dying in his office,” Dr. Whitson says.
Every minute matters after a stroke or heart attack. Speeding up the time from when a patient enters the hospital to when doctors open the clogged vessel and get blood flowing has improved dramatically over the last 20 years. “When you cut the ‘door to balloon’ time, you’re saving lives,” Dr. Whitson says.
Because heart and vascular care has become even more advanced in recent years, nursing has also become more specialized, says Traci Mignery, MS, RN. For example, nurses at the Ohio State Ross Heart Hospital are trained to provide cardiac advanced life support for critically ill patients who may experience complications while recovering from open heart surgery. Nursing units are equipped with instruments that would typically only be in an operating room, so they can initiate bedside emergency care when necessary.
3. Better, easier disease screening
Cardiovascular screening technology has advanced so much that it’s now becoming fast and portable. Patients who would otherwise not even realize they need care are being diagnosed and treated earlier.
“The amount and quality of scans that we can get beamed to our phones and grant access to for patients now is like a sci-fi movie,” Dr. Whitson says.
For example, a portable point-of-care ultrasound (POCUS) system with a Bluetooth-enabled probe provides immediate results to participants at a community health fair or at a mobile walk-in clinic. Care that’s easier to access benefits all patients — especially those living in communities with higher rates of cardiovascular disease and worse outcomes.
Identifying the risks of cardiovascular disease early gives patients the ability to get additional diagnostic screening tests, which are faster and less cumbersome today than in the past.
4. Better preventive medications
Preventive medicine and patient education is also helping patients live longer, healthier lives.
Twenty years ago, there were fewer preventive medications for treating high cholesterol and high blood pressure. “It was just a cookie cutter approach in 2004, but now there’s better awareness that blood pressure control has short and long-term benefits for kidney function, brain function, stroke and coronary artery disease prevention,” Dr. Whitson says.

For patients of cardiologists like Curt Daniels, MD, better diagnostic tests, more access to prevention education and more advanced medicines are contributing to better outcomes against heart disease.
In recent years, there’s been an explosion of whole new classes of cholesterol and blood pressure medications. GLP-1s like Ozempic not only help patients lose weight but also lower the risk of cardiovascular disease.
Doctors and patients are seeing the benefits of preventive medication pay off. Even five years ago, patients in advanced heart failure might have had to consider a device to help their hearts pump blood. Today, those hearts are recovering with new classes of blood pressure medication. “It’s just been a welcome push to try to prevent people from developing these diseases instead of needing big interventions later,” Dr. Whitson says.
5. Genetic information allows for personalized cardiovascular care
Genetic testing has improved the ability to detect and prevent heart or vascular disease. Many patients begin cholesterol or blood pressure medication earlier, based on their lab tests and hereditary risk tests. Patients with a known family history of heart and vascular disease are more likely to be screened for a genetic variant that increases cardiovascular disease risk.
Medication can then be tailored to patients’ specific needs. “We’re looking at the relatives when they’re in their 20s to get ahead of anything there. It just wasn’t part of the conversation 20 years ago,” Dr. Whitson says.
The future of heart and vascular care is moving just as fast
Artificial intelligence (AI) holds promise for exponentially speeding heart and vascular care in the coming years. AI is already helping physicians in their clinics. In the future, nurses at Ross Heart Hospital will use AI’s voice recognition capabilities to assist with documentation, leaving more time for individualized patient care and less time with computer data entry. “Providers can speak out loud as they complete a patient assessment, findings and interventions. The application then documents the care provided in the electronic medical record,” says Mignery.
Providers are also using AI to aggregate massive data sets from patients’ diagnostic tests, lab results and heart monitors. “The amount of data we can look at in a short time would have been impossible to assess all at once. Now it takes five minutes to read it all, which makes it safer and easier for doctors to practice high-quality, safe medicine,” says Dr. Mazzaferri.
Heart disease remains the no. 1 cause of death in the United States, and most people with heart disease eventually succumb to it. But a future without nearly as much heart disease might not be far off, says Dr. Mazzaferri. “In 20 years, it will be a totally different field than what we’re dealing with now.”

Your heart is in the right place
Learn more about advances in care and treatment for patients at The Ohio State University Heart and Vascular Center.
Expert care starts here