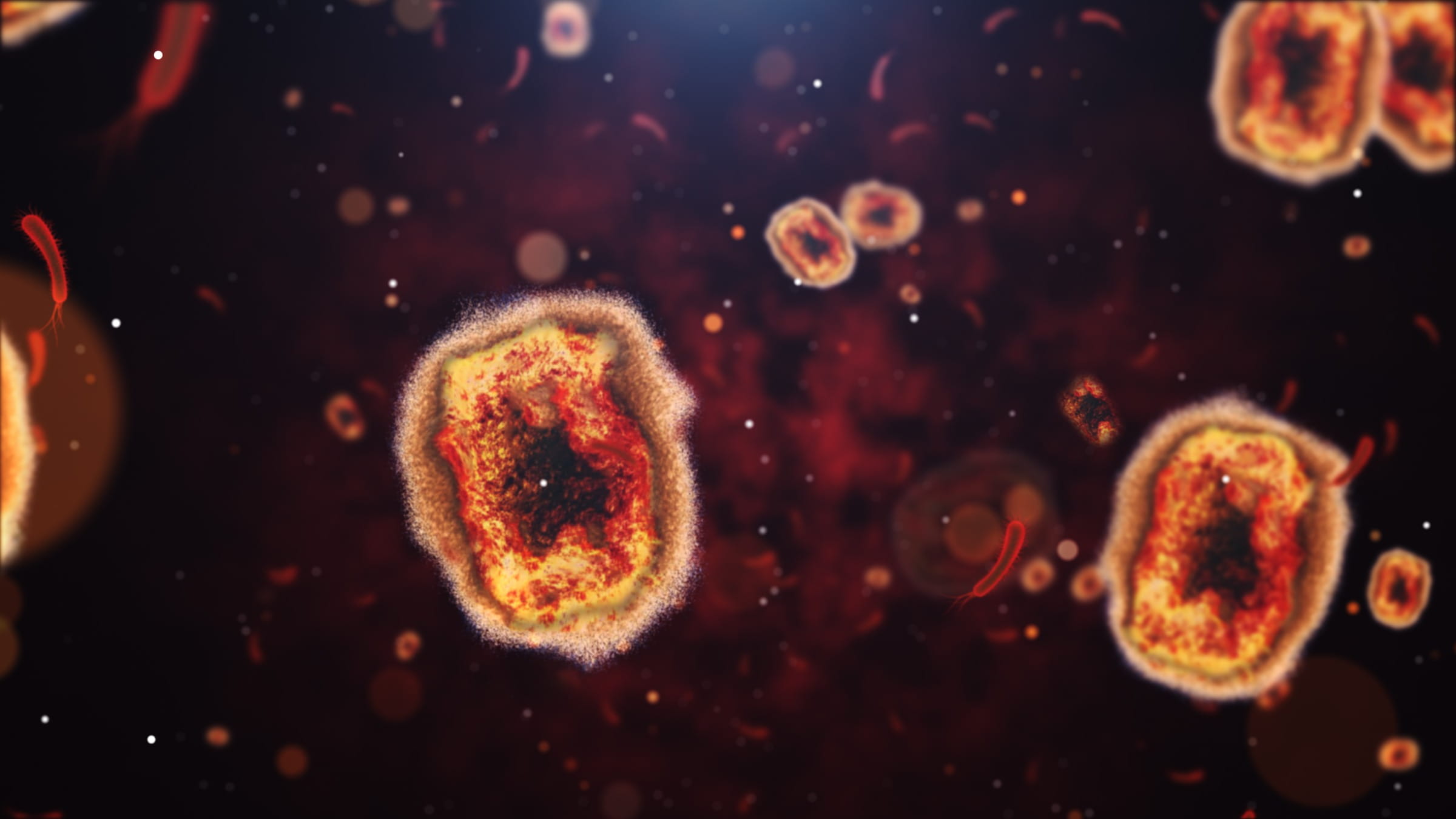
You may have heard about an outbreak of mpox, also known as monkeypox, in Africa, leading the World Health Organization to declare a public health emergency of international concern.
Since January 2023, more than 22,000 mpox cases have been reported in the Democratic Republic of the Congo, and more than 1,200 people have died. Cases are now appearing in nearby countries.
Aug. 14, 2024, an emergency committee of independent experts recommended declaring a public health emergency because the outbreak could spread farther across Africa and to other continents.
What is mpox?
Mpox is a rare disease that was first found in monkeys in 1958 and first recorded in humans in 1970.
The majority of mpox infections are reported in the Democratic Republic of the Congo, with people in several other African countries also having been infected.
According to the U.S. Centers for Disease Control and Prevention says that mpox cases outside Africa are usually linked to international travel or imported animals.
What is the current risk in the United States?
The CDC reports that no known cases of mpox linked to the current outbreak have been found in the United States, and the agency currently considers the risk to the general public in the U.S. to be low.
There has been at least one case reported in Sweden, and the situation is rapidly changing. This latest outbreak is related to a new type, or clade, of mpox spread person to person by close, prolonged direct contact. We may see more cases in more countries in the coming weeks to months.
Has an mpox outbreak ever happened in the United States?
In 2003, there was an mpox outbreak in six U.S. states: Illinois, Indiana, Kansas, Missouri, Ohio and Wisconsin. The 47 cases in humans were all linked to pet prairie dogs that were believed to have been infected when they were housed near other imported, small mammals from Ghana.
In that 2003 mpox outbreak, a joint effort among the CDC, local health departments, the U.S. Department of Agriculture and the U.S. Food and Drug Administration helped contain the disease, ultimately by giving veterinarians and other health care providers plenty of guidance. They used extensive lab testing to confirm cases, and vaccines were available to those at risk. Today, there’s a restriction on imports of rodents from Africa to the United States to further prevent outbreaks like this.
In 2022, a global outbreak led to more than 95,000 cases in 115 countries, including Europe and North America — continents that don’t typically see mpox. About 33,000 cases and 60 deaths occurred in the U.S.
During that outbreak, a new vaccine and treatment were developed. People are higher risk were encouraged to get vaccinated. The vaccine is still available.
Why is the current outbreak of concern?
According to the CDC, the type of mpox currently spreading in Africa typically results in more severe cases and has an increased fatality rate than the type that circulated in 2022.
However, the agency believes that the impacts in the United States would likely be milder.
How is mpox transmitted?
Mpox can be spread from person to person or from an infected animal to a person through bites, scratches, handling wild animals or using products made from infected animals. Mpox can also cross the placenta in pregnancy to a fetus.
When spread between humans, mpox is transmitted mostly through direct contact with body fluids, scabs or infectious sores. It might also spread through materials like clothing or sheets that have touched those body fluids or wounds. If there's long enough face-to-face contact, it can also be spread through respiratory secretions.
The CDC says it’s not yet known if mpox can spread through semen or vaginal fluids, but it can spread during sex and other close contact between people.
According to the CDC, children younger than 15 have been largely affected by the current outbreak. Cases also have been reported among men who have sex with men and female sex workers and their contacts.
However, mpox doesn’t tie itself to any particular group of people, and it can spread between people regardless of their age, gender, sexual orientation or race.
How can I protect myself against mpox?
There’s not proven, safe treatment for mpox right now, but vaccines are available for those who are eligible, based on risk. It’s important to get both doses to ensure protection.
An antiviral drug, called tecovirimat or TPOXX, has been used to treat mpox, especially in people with severe cases or people who are likely to get severely ill.
The safety and effectiveness of the drug is being evaluated through a clinical trial called STOMP. If you or someone you know is diagnosed with mpox, you can find out more about the trial at the STOMP website.
Other ways to prevent mpox
The CDC notes that anyone in the U.S. who has had mpox or is fully vaccinated should be protected. Other ways to protect yourself:
- Avoid close contact with people who have mpox symptoms.
- Avoid contact with materials used by sick people, such as clothing, bedding or health care items.
- Avoid contact with living or dead wild animals.
- Avoid items that have come into contact with wild animals.
- Avoid eating or preparing meat from wild animals or products made from wild animals, such as creams, lotions or powders.
Mpox signs and symptoms
Mpox typically begins with fever, headache, muscle aches and backache, and exhaustion. You’ll also experience swollen lymph nodes.
Within about one to three days after fever begins, a rash develops, often beginning on the face and spreading to other parts of the body. Illness usually lasts two to four weeks.
If you develop those symptoms, you should contact your health care provider. For more information and updates on mpox outbreaks, you can visit the CDC’s informative page on the virus.





