Imaging the future: Ohio State researcher brings new cardiac imaging technology to the masses
Orlando Simonetti, PhD, has pioneered the field of cardiac imaging and is now unveiling a rare type of MRI scanner that promises to expand cardiac MRI access for thousands of patients.
Over the past 30 years, heart and vascular researcher Orlando Simonetti, PhD, has played a pivotal role in the effort to bring cardiac MRI technology into the mainstream. Now, as The Ohio State University Wexner Medical Center unveils a rare type of MRI scanner, he looks forward to expanding cardiac MRI access for thousands of patients, including his own wife, Lynn.
In early 2017, Lynn Simonetti was diagnosed with dilated cardiomyopathy and heart failure. One of medicine’s most powerful diagnostic imaging tools, magnetic resonance imaging (MRI), played a key role in establishing a diagnosis. Unfortunately, severe claustrophobia made the diagnostic process unbearable.
“When I was put into the MRI that they usually use for cardiac images, I screamed, ‘Get me out of here! I can’t do this,’” she remembers.
Lynn was eventually able to undergo the MRI in a somewhat larger machine at the Ohio State Wexner Medical Center, but she could only tolerate it with a cloth over her eyes. While her heart function has improved substantially since her initial diagnosis, she still requires periodic MRIs to monitor her condition. But going forward, claustrophobia isn’t the only downside of undergoing these tests. Because she now has an implanted metal device, the image quality of her MRI scans will be worse than before.
Someone needed to make MRI more accessible and effective for a broader range of patients. Ironically, that someone was Lynn’s husband, Orlando Simonetti — the John W. Wolfe Professor in Cardiovascular Research at The Ohio State University College of Medicine and one of the leading contributors to the field of cardiac imaging. Through decades of pioneering breakthroughs, Simonetti paved the way for the creation of a machine that illustrates the untapped value of low-field (low magnet strength) MRI for imaging cardiac patients like his wife and introducing new procedures, such as MRI-guided cardiac catheterization, as a radiation-free alternative to other forms of cardiac imaging.
Simonetti shared his vision and research surrounding the potential for low-field cardiac MRI with Siemens Healthineers, which released the 0.55T MAGNETOM Free.Max in late 2021. Now, as the Ohio State Wexner Medical Center becomes one of the first hospital systems in the country to introduce patients to the 0.55T, Simonetti looks back at the career milestones that led him to this point and forward to the limitless potential of cardiac imaging.
Laying a Foundation
Like many scientists, Simonetti happened upon his area of study by chance.
He remained at Ohio State after his undergraduate years to earn a master’s degree in biomedical engineering, which he considered an ideal blend of hard science, math, physics and biology. He then returned to Cleveland, his hometown, to work as a computer systems analyst at Case Western Reserve University. A lover of learning by nature, he took advantage of the tuition benefit offered to university employees and began to think seriously about pursuing a PhD.
At the same time, a close friend he met at Ohio State, Jeffrey Duerk, PhD, accepted a faculty position at Case. In 1989, Duerk asked Simonetti to join his lab, which focused on improving MRI technology by designing imaging techniques to be less sensitive to motion.
MRI scanners, which first appeared in clinical settings in the early 1980s, use magnetic fields and radio waves to create detailed images of the body and diagnose disease. The permanent magnet in the MRI machine creates a magnetic field in the body, while the application of radio waves causes the body’s hydrogen atoms to deviate from the magnetic field. When those radio waves are turned off, the hydrogen atoms realign with the magnetic field and produce signals that the MRI’s computer software can use to generate an image.
Though cardiovascular magnetic resonance imaging (cardiac MRI) was mostly uncharted territory in the 1980s, researchers recognized the technology’s potential for assessing the function and structure of the heart and blood vessels in a noninvasive way, making it possible to diagnose conditions like coronary artery disease, congenital heart disease and diseases of the heart muscle.
Cardiac MRI carves out new pathways for diagnosing disease that complement other imaging techniques. Consider cardiac computed tomography (CT), a commonly used imaging test that uses X-rays to take pictures of the heart. On one hand, cardiac CT produces very high-resolution images of the coronary arteries and blood vessels that are superior to MRI. On the other hand, cardiac MRI paints a more detailed portrait of the structure and function of the heart muscle, the myocardium. MRI is also free of radiation, avoiding the exposure to radiation that accompanies cardiac CT.
Echocardiography, a form of medical imaging that uses sound waves to create moving pictures of the heart, is used frequently as first-line cardiac imaging. An echocardiogram machine is significantly more portable and available than an MRI and provides real-time images of the moving heart and blood flow. Ultimately, though, the MRI can uniquely evaluate the heart muscle in ways that echocardiography and CT cannot, making MRI the gold standard of cardiac imaging for the foreseeable future.
While MRI technology has revolutionized the field of medical imaging over the past 40 years, there were major wrinkles to iron out in the early days.
“Back then, MRI scans were much slower, making cardiac imaging especially problematic due to the motion of the heart,” Simonetti says. “The image quality today is night and day from what it was.”
For Simonetti and his fellow researchers, creating a clear image of a beating heart was easier said than done. “Though we developed relatively crude ways to image the heart in the 1980s, it wasn’t until MRI hardware improved in the late 1990s that we really started to witness breakthroughs in the field of cardiac MRI,” he says.
With characteristic modesty, Simonetti fails to mention that he was a central driver of many of these breakthroughs. In 1992, he accepted a scientific development role at Siemens Healthcare, rising to the position of director of Cardiovascular MR Research and Development. For more than a decade, he led a team in writing pulse sequence programs. “We programmed the MRI machine to make images sensitive to things like scarring, blood flow and excess fluid in the heart muscle,” he explains. “You have to be a physicist, a physiologist and a programmer to put it all together.”
In 1997, the future of cardiac MRI changed overnight when Siemens released a new MRI platform with tremendous improvements in imaging hardware and a more flexible software platform.
In his 13 years at Siemens, Simonetti and his team made technological advances that still set the gold standard for cardiac MRI today. “He has developed sequences that are still being used clinically all over the world,” says Rizwan Ahmad, PhD, an assistant professor of biomedical engineering at the Ohio State Wexner Medical Center. “It’s hard to overstate how well-respected and well-established he is within the cardiac MRI community.”
Within the field of medical imaging, Simonetti is best known for his role in inventing a technique called late gadolinium enhancement (LGE). LGE provides an unprecedented view of scarring and fibrosis — the development of fibrous connective tissue in response to damage — in the myocardium, the muscular tissue of the heart. To this day, his seminal paper on the inversion recovery LGE pulse sequence is one of the 100 most-cited articles in medical imaging literature.

Putting the pieces together
In 2005, Simonetti was scanning the horizon for new opportunities to translate cardiac imaging research into clinical impact. He didn’t have to look any further than his alma mater, which had recently established the Richard M. Ross Heart Hospital and the Dorothy M. Davis Heart and Lung Institute, “sister” facilities on the same campus that provided a direct connection between researchers and clinical care.
“I’m a Buckeye through and through, so when I heard they were recruiting a director of cardiac MRI research, I jumped at it,” he says. “As a major bonus, they were installing a new Siemens MRI machine in the Ross Heart Hospital dedicated to cardiac imaging, which was almost unheard of at the time.”
Today, Simonetti, who holds the John W. Wolfe Professorship in Cardiovascular Research at Ohio State, is an integral member of a group of researchers and students within the Ohio State colleges of Medicine and Engineering who are dedicated to cardiac imaging. To date, the imaging techniques and technologies they have created are linked to at least 25 patents.
“A major part of what we do is come up with new ways to solve problems, and if something is unique enough, we can patent it,” he explains.
One major contribution of this team, a technique called myocardial T2 mapping, offers a way to detect edema — excess fluid buildup — and inflammation in the myocardium. Previous techniques failed to detect these conditions with enough accuracy to be useful in a clinical setting, but the team built upon previous research to create a robust, reliable, quantitative method to detect and gauge the severity of inflammation in the heart.
In the past two years, myocardial T2 mapping has played an essential role in safeguarding the health of athletes who have contracted COVID-19, which can cause myocarditis — inflammation of the heart muscle. In a protocol that has now been adopted by every school in the Big Ten Conference, every athlete at Ohio State who tests positive for COVID-19 undergoes a cardiac MRI before being cleared to return to strenuous activity.
Another major area of research for Simonetti has been the development of methods to image the heart under conditions of exercise stress. Typically, patients with chest pain symptoms undergo stress tests using treadmills and other exercise equipment. These stress tests give physicians the ability to look at changes in the electrocardiogram (ECG) that can distinguish heart disease from other causes of symptoms. While MRI can offer superior image quality to aid in diagnosis, the magnetic components of exercise equipment are not compatible with the magnetic field of the MRI machine. For this reason, MRI stress testing is performed almost exclusively with stress-inducing drugs rather than the more natural method of exercise stress.
Simonetti reached out to John Arnold, a hydraulics expert at The Ohio State University College of Food, Agricultural, and Environmental Science, to help him design an MRI-compatible treadmill with a hydraulic motor and nonmagnetic materials.
“That’s one of the greatest advantages of Ohio State,” Simonetti reflects. “You can find an expert in just about anything here.”
The MRI-compatible treadmill can be positioned right next to the patient table, allowing the patient to quickly and safely transfer to the MRI scanner immediately after exercise, while the heart rate is still at its peak.
At Ohio State, one of these MRI-compatible treadmills is currently in use at the Ross Heart Hospital, with a second machine in use at the new Advanced Cardiac Imaging Center that recently opened at the Martha Morehouse Outpatient Care Center. Together with his colleagues in cardiovascular medicine, Simonetti ran two large clinical trials at six different sites, publishing the results to illustrate the potential of MRI-compatible exercise equipment. The field of exercise stress MRI continues to evolve, with other devices now available for patients to exercise while lying in the MRI magnet.

Expanding the realm of possibility
While innovations like myocardial T2 mapping and MRI-compatible exercise equipment have already impacted thousands of lives in Ohio and beyond, Simonetti now focuses much of his time on improving technology with even greater potential for large-scale impact: low-field MRI.
MRI field strength, which describes the strength of an MRI magnet, is measured in Tesla, or “T.” While MRI started out using relatively low-field magnets, the technology has gradually evolved toward a “bigger is better” mentality that prioritizes the development of higher and higher field MRI machines, now ranging as high as 11T. The reasoning goes that with higher strength comes more signal, more detail, faster scanning and less noise — not audible noise, but a kind of disruption of the image. “You can think of noise like snowflakes on the TV screen, obscuring the underlying picture,” Simonetti explains.
But while high-field strength has some advantages over low-field — in particular, the clear, high-resolution images it can produce — bigger isn’t necessarily better for every clinical case. High-field MRI can be of little or no value in patients with implanted devices because of the way metal distorts MR images, and it’s not useful for imaging the lungs. For obese or claustrophobic patients, the narrowed bore of high-field MRI machines leave them searching for alternative options. And these machines are also heavier and more expensive than low-field counterparts, limiting their use in regions of the world where medical institutions may not have the financial resources to acquire, house and maintain them.
Ahmad remembers attending a conference with Simonetti in 2015 where they Iistened to presentations about an ultra-high-field 7T machine. “The whole time, we were thinking, ‘That’s great, but how many institutes can actually afford a 7T?’” Ahmad says.
“We were interested in looking at the other end of the spectrum to make cardiac MRI more affordable on a global scale. That’s where low-field MRI comes in.”
Simonetti and Ahmad knew that if they could develop software techniques that suppressed noise in low-field MRI, they could expand access to cardiac MRI for patients at home and across the globe. Determined to give it their best shot, they identified a medical technology company in Cleveland called ViewRay that agreed to let them run experiments on its 0.35T MRI machine, a significantly lower field machine than the 1.5T in use at the Ross Heart Hospital.
After a period of testing and experimentation, they succeeded in producing high-quality, low-noise images of the heart that resembled those produced by a much stronger MRI machine. “We demonstrated that with powerful processing techniques, we can still get diagnostic quality images using weaker hardware,” Ahmad says.
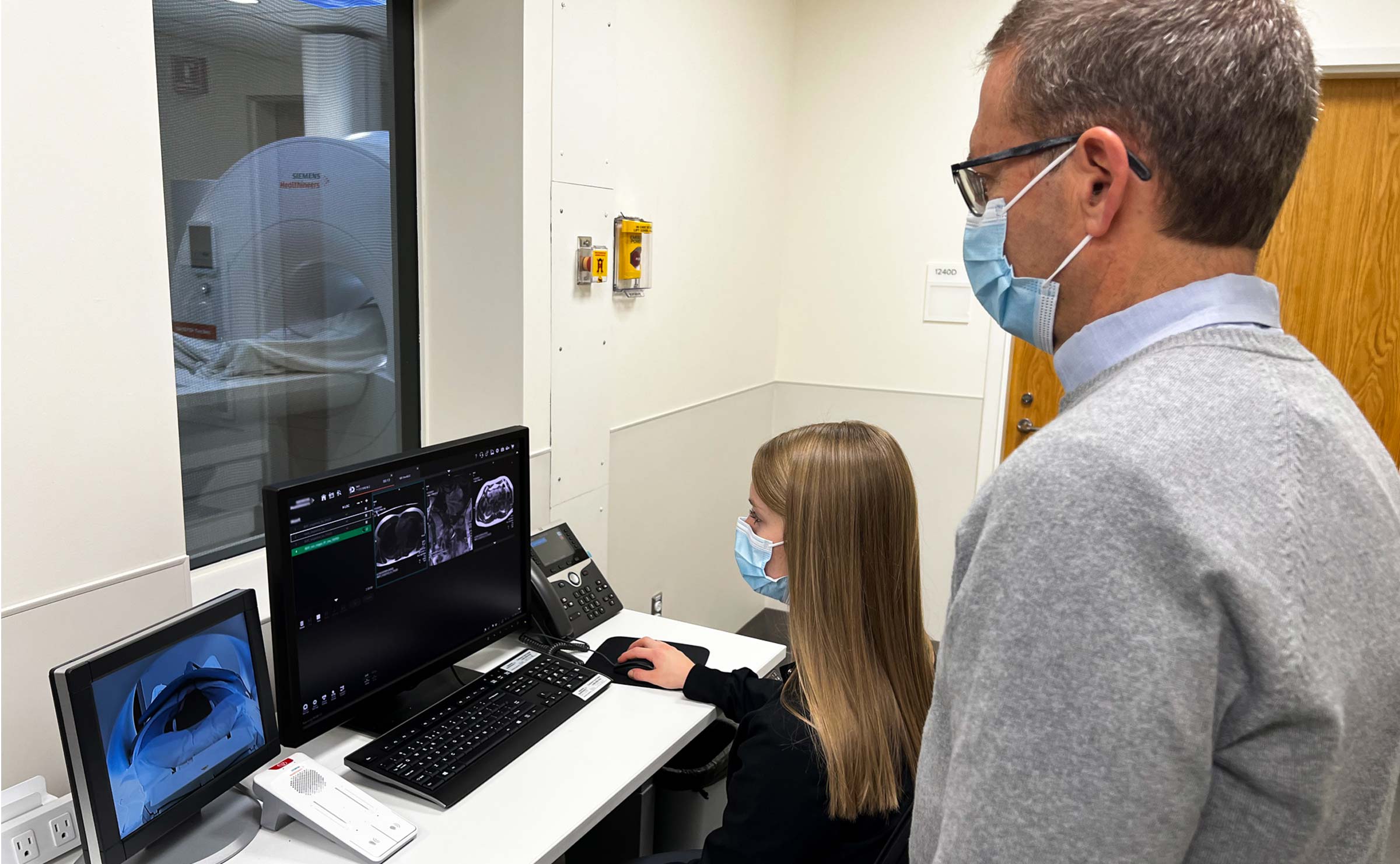
After attaining proof of concept and publishing a paper on their findings in 2017, the pair of researchers shared their vision with Siemens. Over the next few years, Siemens produced the commercial 0.55T system that was installed at the Ohio State Heart and Vascular Center in November 2021. The 0.55T is currently being used for research purposes as Simonetti and Ahmad work with Siemens to build cardiac imaging techniques for the machine in the same way they built techniques for the 0.35T.
Simonetti anticipates the 0.55T will be ready for clinical use in spring 2022, along with the recently acquired 3T machine installed alongside it. From his perspective, having three different magnet strengths available to the Ohio State Heart and Vascular Center imaging program — 0.55T, 1.5T and 3T — provides an unparalleled level of flexibility in diagnosing cardiac patients. “It’s a rare thing to have three different field strengths within the same institution,” he says. “Our intention from both research and clinical perspectives is to take advantage of this unique opportunity to put the right patient in the right machine to get the best outcomes.”
Introducing the 0.55T
Simonetti is quick to emphasize that just like with different forms of cardiac imaging, each MRI field strength has distinct advantages. Depending on specific patient characteristics or diagnostic questions, he may turn to high-, medium- or low-field strength. At the end of the day, higher-field machines still offer the highest possible resolution and higher speed scanning, but they’re not right for every application.
The practical advantages of adding the 0.55T to the mix are immediately evident to those familiar with high-field MRI technology. For one thing, the 0.55T scanner weighs and costs significantly less than higher-field counterparts and consumes fewer resources to operate. Compared to a conventional 1.5T or 3T scanner, which use 1,000 to 2,000 liters of liquid helium to keep the magnet cold, the 0.55T magnet only uses 0.7 liters. Its larger opening — 80 centimeters compared to the standard 60-70 centimeters — also expands access for patients who are obese or claustrophobic. Recently, Simonetti obtained funding from the National Institutes of Health to develop cardiac imaging on the new 0.55T system for severely obese patients in collaboration with Ohio State heart failure specialists, as well as Sabrena Noria, MD, PhD, at the Ohio State Wexner Medical Center’s Comprehensive Weight Management Program.
While Simonetti is primarily focused on cardiac imaging, the 0.55T will also open the door to lung imaging because the signal from the lungs — a mix of air and tissue — is actually higher at lower-field MRI. Perhaps most significantly, the 0.55T MRI creates a safe environment for the development of MRI-guided interventional cardiology procedures, which are currently incompatible with higher-field machines that can overheat the wires used on these procedures.
In partnership with interventional cardiologist Aimee Armstrong, MD, at Nationwide Children’s Hospital, as well as companies that manufacture interventional devices like catheters and stents, Simonetti will investigate the potential to perform cardiac catheterization procedures in the 0.55T scanner. Catheterization involves guiding a thin, flexible tube through a blood vessel to the heart to diagnose or treat conditions like arterial blockages or irregular heartbeat. Children who live with congenital heart disease undergo repeated heart catheterizations over the course of their life, he points out, and the 0.55T provides a radiation-free alternative to conventional procedures that require X-ray guidance.
Patients with medical devices like pacemakers and defibrillators will also benefit from the 0.55T machine. The metal in these devices always distorts the magnetic field used to form images, but this distortion is worse at higher field strength. Using their noise-suppressing software techniques, Simonetti and Ahmad hope to take advantage of the reduced distortion at low field and use the 0.55T machine as the technology of choice for patients with implanted devices.
In addition to all these advantages, the affordability of low-field MRI expands the realm of possibility for diagnostics and treatment in less resource-rich countries and regions, according to Yuchi Han, MD, who became the Ohio State Wexner Medical Center’s new director of cardiac imaging in October 2021. Though certain diagnostic questions are best answered by high-field MRI, a low-field MRI scanner may be all that many medical institutions can afford. “Dr. Simonetti’s efforts are making this technology more accessible on a global scale,” Han says.

A life’s work hits home
From innovations like myocardial T2 mapping to ongoing work on low-field MRI scanners, Simonetti has constructed many of the foundations of the modern-day cardiac imaging field. As one of cardiac MRI’s most prolific researchers, he has directly impacted countless lives around the globe.
At the same time, his efforts are also making a difference closer to home.
Between her pacemaker and her severe claustrophobia, Lynn Simonetti is an ideal candidate to undergo continued monitoring on the 0.55T. “I think the 0.55T will help a tremendous number of people,” she says. “There are a lot of people who have pacemakers like I do, and the images with this new machine will be better for people with implanted devices. And the opening is quite a bit bigger, so I’m looking forward to not being as anxious about being in the MRI.”
While Lynn has always supported her husband’s career, her experience imparted a newfound appreciation for him and his colleagues. “I knew that he was helping cardiac patients, but to actually become one of those patients and benefit from what he and other researchers have developed has been amazing,” she says.







