Surgical team makes Ohio State a destination for treating rare, difficult skull-base tumors
Team pioneers and trains surgeons around the world on this life-changing procedure
For Diana Robertson, the pain was sharp and constant.
“It’s always there. It always hurts, all the time. That never goes away,” she said the morning she arrived for brain surgery at The Ohio State University Wexner Medical Center.
Robertson, 59, of Mansfield, Ohio, suffered through debilitating headaches for 10 years.
“It gets excruciating” she said, describing the unrelenting, sharp sensation behind her temples.
The culprit was a benign tumor lodged inside a pituitary gland in her brain.
Fortunately for Diana, a pair of surgeons who were among the first in the world to pioneer a minimally invasive surgical technique for these rare and difficult-to-treat tumors were waiting for her at the Ohio State Wexner Medical Center.
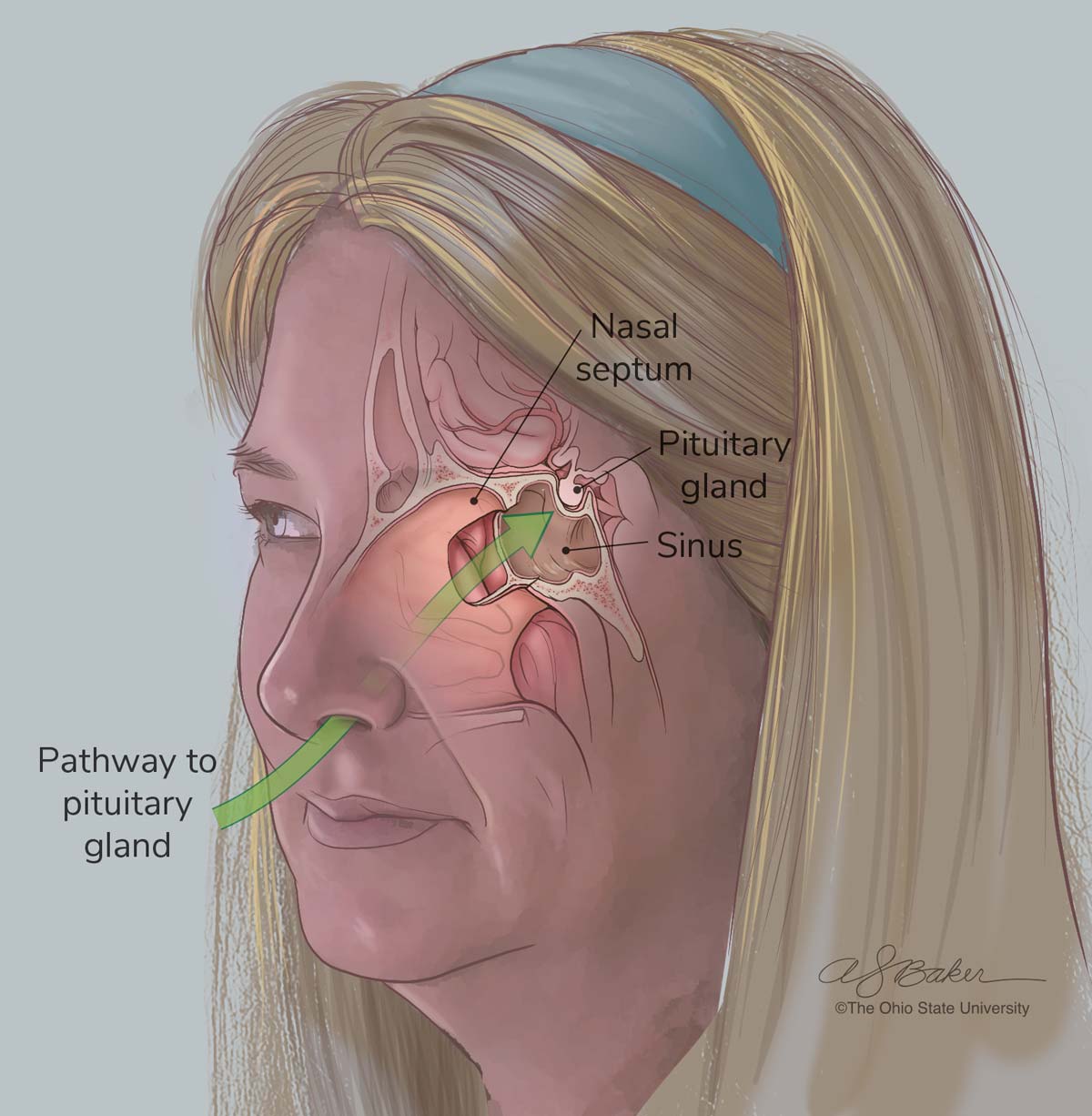
Daniel Prevedello, MD, a neurosurgeon, and Ricardo Carrau, MD, an otolaryngologist-head and neck surgeon, have worked together for decades at the Ohio State Wexner Medical Center and The Ohio State University Comprehensive Cancer Center – Arthur G. James Cancer Hospital and Richard J. Solove Research Institute (OSUCCC – James), to perfect the techniques of endoscopic endonasal surgery, a procedure in which brain tumors are removed through the nasal passageways instead of through an open incision in the patient’s skull. It requires both of their unique skillsets — one with the skill to traverse the intricacies of the brain and one with the skill to navigate the complex and delicate passageways of the nasal system.
During the dozen or so years they’ve been practicing at Ohio State, Drs. Prevedello and Carrau have made the medical center a destination for removing some of the world’s riskiest and challenging skull base tumors.

Taming a “very complicated beast”
Surgeries within the skull base are inherently high risk. The skull-base area is described by surgeons as a “salad bowl” that the brain sits in. The spinal cord and surrounding nerves run through a hole at the base of the bowl. The skull base is the nexus of where many nerves, arteries and sensory organs intersect behind the nasal cavity.
 There’s no room for error when surgeons remove invasive tumors.
There’s no room for error when surgeons remove invasive tumors.
“That area is a very complicated beast,” says James Rocco, MD, PhD, chair of the Department of Otolaryngology – Head and Neck Surgery at the Ohio State Wexner Medical Center.
“Arguably, it’s one of the most complicated anatomical areas of the body with grave consequences for errors. An error with a blood vessel can lead to a stroke and death,” Dr. Rocco says. “A little error with a nerve can lead to blindness, a loss of sense of smell, or affect your facial movements or make it so you can’t eat or swallow.”
It takes a certain personality type to routinely perform high-risk surgeries.
“You go to the edge of risk in order to help people and there’s a personality behind that because not everybody can deal with that every day,” Dr. Prevedello says. “But you do see improvement immediately. There are some patients who are losing vision because the tumor is pushing on the optic nerve.”
More than 10,000 Americans are diagnosed with pituitary tumors like Diana’s each year, according to the American Cancer Society.
Cancerous brain tumors in the skull base are exceptionally rare. Head and neck cancers account for 4% of all cancers in the body. Of those, 0.01% are located in the skull base.
Finding a surgeon who has had significant experience removing these types of tumors can be challenging.
Dr. Prevedello, a professor of Neurological Surgery at the Ohio State College of Medicine, is one of only a few neurosurgeons in the world who have performed more than 1,500 endoscopic endonasal approach surgeries. Dr. Carrau, a professor of Otolaryngology at the Ohio State College of Medicine, has completed an estimated 2,000 endoscopic endonasal approach surgeries in his career.
Pioneering minimally invasive neurosurgery to treat skull base tumors
“I started developing the endoscopic endonasal surgery techniques in the 1990s with a neurosurgeon at the University of Pittsburgh,” says Dr. Carrau, who was on the Pittsburgh faculty at the time.
“We developed techniques in our head and then did some lab work to see if that would be feasible,” he says.
Rather than opening the skull to remove tumors, Dr. Carrau began developing an approach using an endoscope through the nasal passageways to gain access to the central part of the skull base.
The technique, which proved successful, meant a quicker recovery time for patients with no oral or outside facial or head scarring.
Dr. Prevedello was a neurosurgery fellow in the mid-2000s in Pittsburgh. The pair met and began working together in what would become a decades-long partnership.
“So he participated actively in the development of some of these techniques, and they have continued to be fine-tuned, and we have developed others along the way,” Dr. Carrau says. “But for the most part, that was the birth of what we call endoscopic skull base surgery.”
Before this technique, the surgery frequently was incredibly invasive with a lengthy recovery for patients.
Patients would have part of their head shaved. A craniotomy would be performed, creating a long incision across the top of the head stretching from ear to ear.
“They would essentially peel your face down below your eyes and then drill through the brow bone here,” Dr. Rocco says gesturing to his brow. “They would push the brain back and then operate on the salad bowl.”
That highly invasive surgery was riskier for patients. Just pushing the brain back to access the skull base would result in about a 7% death rate.
“What Ric (Carrau) figured out is he could take these new techniques we were using for endoscopic sinus and apply them to the skull base.,” Dr. Rocco says.
Endoscopic surgeries don’t work for all brain tumors.
“There is a limitation of what we can do through an endoscope,” Dr. Carrau says. “If the tumor is attached to a main vessel, or maybe some nerve, it may not be the best approach. If it crosses too much to the sides of the eyes, obviously we cannot reach it in the same way. We cannot tackle every tumor that way, but we can tackle a good portion of them.”
Easing pain for the patient and shifting more of the burden to the surgeon
With the endonasal approach developed, neurosurgeons had to re-think how they approached tumors. They were used to approaching the surgery from the top of the skull. Now they had to start accessing the skull base through the bottom up through the narrow corridor of the nasal passages.
“You’re trying to do the same type of surgery that originally was performed with large openings where you can see and have plenty of space to move. Now you’re trying to go through a small corridor and the freedom of movement is not there,” Dr. Prevedello says.
The surgeries last hours and require exceptionally fine and precise movements to prevent damage to surrounding crucial structures. By doing that, surgeons often put themselves in awkward positions for long periods of time that can cause hand cramps, fatigue and backaches.
“We like to say that in general, we have been transferring the pain from the patient to the surgeon, because that’s what happens,” Dr. Prevedello says.
“You have difficulty to go through, but once you’re able to get that tumor out, the patient is so grateful. That’s what makes us keep going in minimizing the invasiveness of the approach. This is our motivator.”
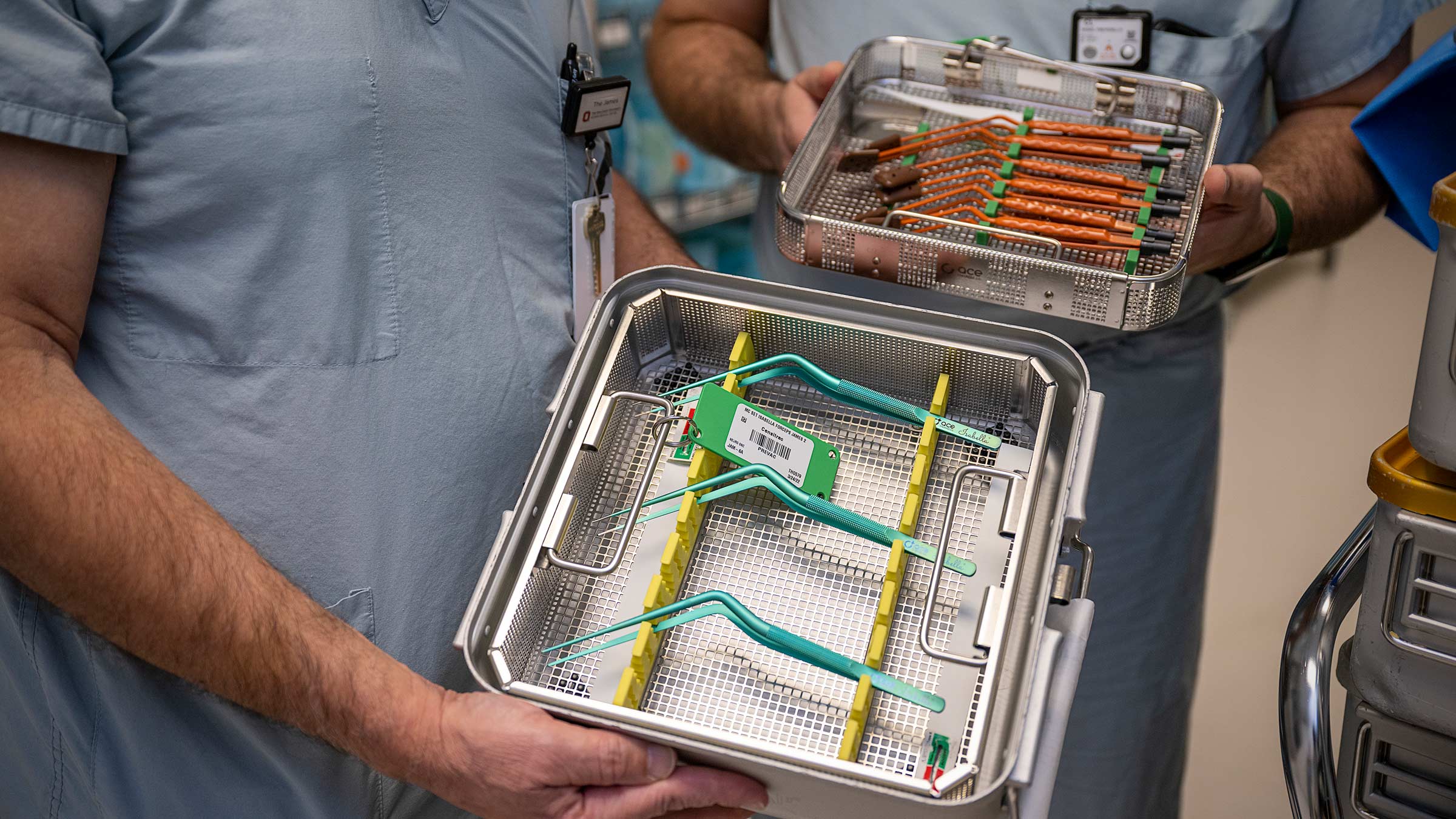
Over time, Dr. Prevedello invented several surgical tools to make operations go smoother.
“We invented ergonomic sections,” Dr. Prevedello says. “We combined the nicknames of Ric’s daughter, Didi, and one of my daughters, Bella. We call them Di Bella sections.”
It’s one of several instruments they’ve developed.
“They have the same shape to not fight with the endoscope when we go through the nostril. So that’s kind of my contributions to the field,” Dr. Prevedello says. “A lot of people use this dissector because they see me working and they don’t see me struggle. It’s very helpful, like having those specific angles that we designed.”
Ohio State: A destination for some of the most challenging tumors in the world
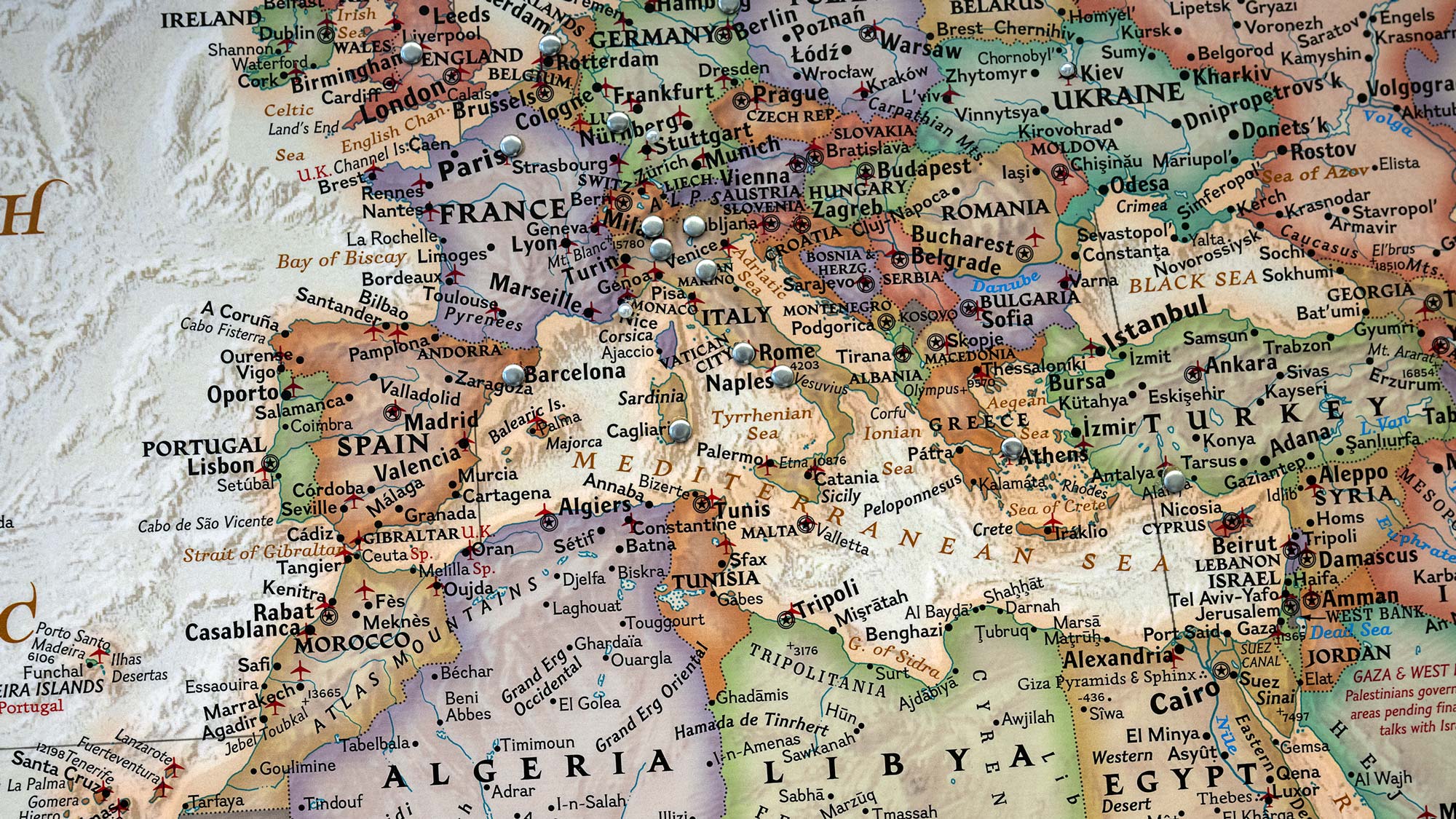
A large world map is posted behind Dr. Prevedello’s desk inside his office at the OSUCCC – James with pin marks scattered across continents.
The pins mark locations where Dr. Prevedello has performed neurosurgeries and demonstrations. Remote parts of Russia in Siberia, India, Italy, Costa Rica, Colombia, Thailand, Brazil and Dominican Republic are among the locations pinned.
“Because they’ve been doing it for so long, and because they’ve been working together as a team, they really became the world’s experts,” Dr. Rocco says. “They’ve traveled the world to teach people how to do this.”
There’s a highly competitive skull-base fellowship in both neurosurgery or otolaryngology specialties that pairs up a fellow with Drs. Prevedello or Carrau for a year to learn and perfect the techniques.
There are also a limited number of research fellowships available as well as a visiting scholars program. Visiting scholars, who are often sponsored by their hospital or government, stay at Ohio State anywhere from six months to two years and work in the surgical anatomy lab to evolve their surgical techniques.
“We won’t be here in the future. It’s very important that this continues. I think this really is motivation for us,” Dr. Prevedello says.
Since they arrived at Ohio State, the surgical skull base program has doubled in capacity to care for more patients. Now there are two teams of surgeons who can work interchangeably when patients need surgery.
Each year the skull base program performs more than 200 endoscopic surgeries. Patients sometimes cross the globe seeking the pair’s expertise.

Teaching a choreographed dance in the operating room
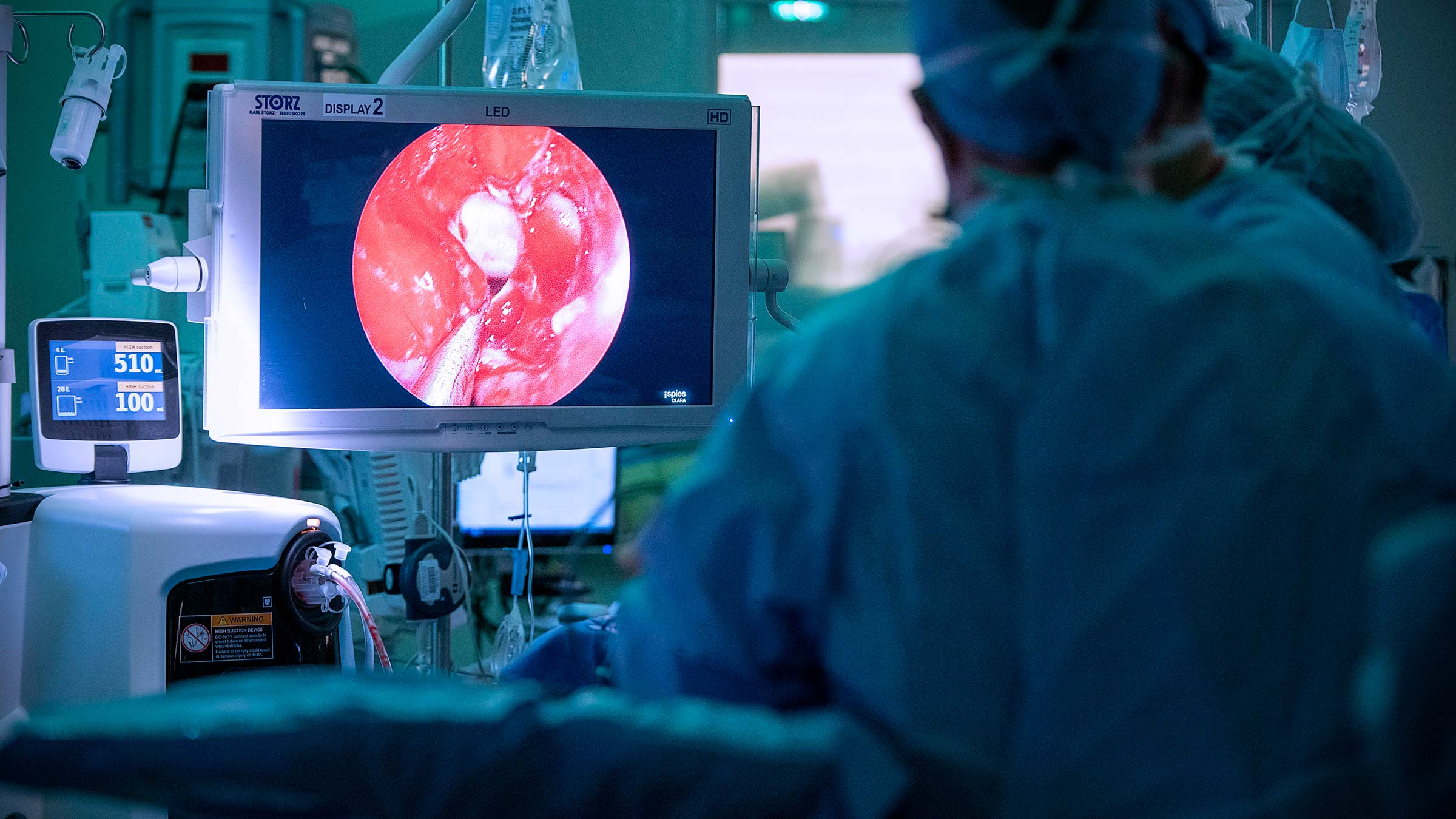
The morning of Diana’s surgery, a packed auditorium of surgeons was shown her MRI and imaging slides on screen as part of a three-day course run by Drs. Prevedello and Carrau. Diana’s surgery would be showcased live to the waiting auditorium.
Dr. Carrau narrates the surgery from the operating room. Even before a single incision is made, there are so many details to consider. Surgeons have to know how to position the patient, where does Dr. Prevedello stand in relation to Dr. Carrau when they’re operating together and what position allows for less cramping for the surgeons’ hands?
“Elevating the head of the patient is going to decrease the bleeding related to the capillary. We have the head kind of tilted to the left and turned to the right a little bit,” he says to the audience, noting where Dr. Prevedello’s hands will go during the surgery and where he will initially stand in relation to Diana’s head.
Dr. Carrau starts clearing a pathway through the nasal passages using small surgical scissors. He’s taking down a wall, entering the sphenoid sinus, which is a nasal sinus area behind the nose between the eyes.
“Some people like to do the tissue this way, in kind of a flicking motion,” Dr. Carrau says. “I like to continue taking it out in a way that looks like I’m erasing or painting the tissue. The advantage that I find is that I’m removing the tissue all the time as opposed to half of the time. But again, completely personal preference.”
When Dr. Carrau completes the opening, the carotid arteries, optic nerves and pituitary gland are accessible.
There’s little to no room for errors when surgeons remove invasive tumors.
Drs. Carrau and Prevedello’s choreography in the operating room tells the story of their enduring partnership and trust in one another.
“What makes this really special is that Prevedello and Carrau have to function like dance partners that coordinate moves in perfect sequence. And I’ve asked them, ‘Don’t you get tired of operating together all the time?’” says David Cohn, MD, interim chief executive officer and chief medical officer at The James Cancer Hospital and Solove Research Institute.
Colleagues take note of the pair’s professional relationship and friendship.
“It’s almost like a marriage, right? Just how interactive they are with each other in the operating room, Dr. Rocco says. “It’s unspoken. I think they’ve just been through so much together and their surgical experiences are unparalleled in the world. They are the leaders.”
During Diana’s surgery, the audience of surgeons erupts in applause as Dr. Prevedello removes the last piece of her tumor.
“There it is — it’s a huge piece,” Dr. Prevedello says after dissecting the back wall of the grape-size tumor from Diana’s brain. He asks the audience if there are any questions. Not for the moment. His fellow surgeons are in awe.
Diana’s vitals are measured by a rhythmic monotone pattern beeping in the background. The vacuum noise of suction sounds periodically. Like the pair have done a thousand times before, they work in tandem to close and rebuild the nasal passageway after removing the tumor.

Waking up from a nightmare of never-ending headaches
Within a day of waking up from surgery, Diana noticed something was different. While her nasal passageway and sense of smell would take a few months to heal, she noticed something else was missing.
The dull head pain that had plagued her for a decade had vanished. The ache behind one of her eyes had disappeared.
“I felt off. I didn’t feel normal because the headache became part of who I was. It had been there so long,” Diana says.
Three months later when she visited Dr. Carrau for her last checkup with him, she was more outgoing. A smile stretched across her face. Even her voice seemed less strained.

In an exam room she choked back tears of relief. “I try to apologize to everybody now. Because I’m realizing how it affected my mood and how irritable it made me all the time.”
Before, she wasn’t able to tolerate the pain and actively play with her grandchildren.
Since her surgery, they’ve had outings to the park, jumped on the trampoline and she hosted a carnival-themed birthday party for the youngest grandchild.

“The doctors are amazing. Everyone here has been amazing. They know what they’re doing. I have confidence in them,” Diana says.

Move forward with confidence
Get clarity with an online second opinion for cancers.
Get an online second opinion




