
Rebuilding your life after an accident or other traumatic event is possible
Our nationally ranked team can help you recover.
Learn more Your source for health, wellness, innovation, research and science news from the experts at Ohio State.
Your source for health, wellness, innovation, research and science news from the experts at Ohio State.
There’s a powerful story behind every headline at Ohio State Health & Discovery. As one of the largest academic health centers and health sciences campuses in the nation, we are uniquely positioned with renowned experts covering all aspects of health, wellness, science, research and education. Ohio State Health & Discovery brings this expertise together to deliver today’s most important health news and the deeper story behind the most powerful topics that affect the health of people, animals, society and the world. Like the science and discovery news you find here? You can support more innovations fueling advances across medicine, science, health and wellness by giving today.
Subscribe. The latest from Ohio State Health & Discovery delivered right to your inbox.
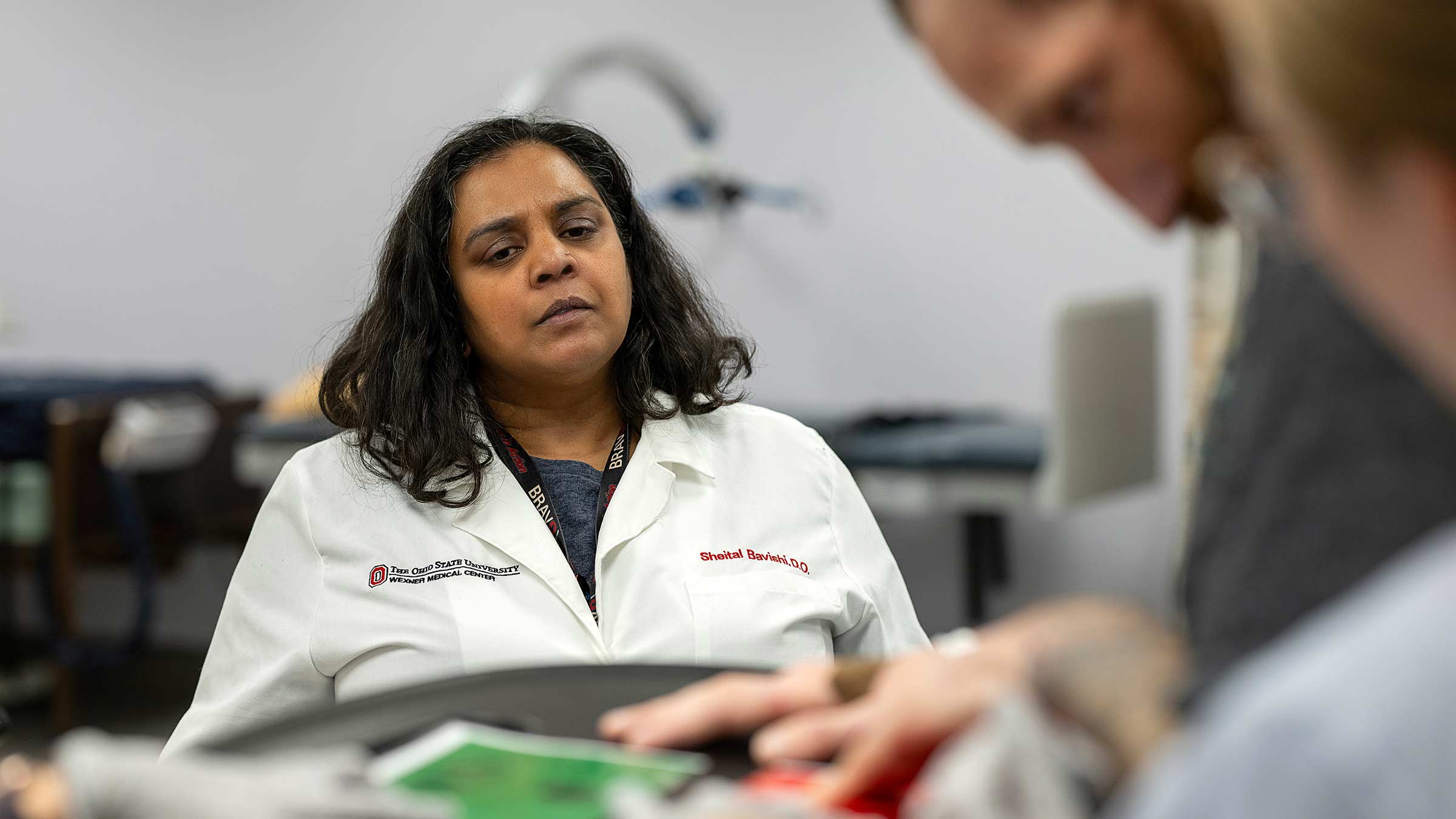
SubscribeSheital Bavishi, DO, started Ohio’s first program offering intensive therapy to awaken patients from comas after severe brain injuries.
Before therapists ask TJ Niebel to draw a line, they remind him:
You’re here at Ohio State. You’re here in the hospital. You had an accident on your ATV. But you’re safe now. You’re in physical therapy and speech therapy. It’s Monday afternoon.
Katie Krumpak, MA, MBA, puts a marker in TJ’s left hand, his writing hand. He holds the tip of the pen a couple of inches above the dry-erase board and keeps it there.
“Can you draw a line?” asks Krumpak, a speech pathologist at The Ohio State University Wexner Medical Center.
He stays still until Krumpak moves his hand, putting her hand on his to draw a line.
“Like that.” She lifts her hand. “Now you do it.”
His hand shakes. Eventually he lowers the tip of the pen onto the board to draw a short squiggly, red line.
“Nice job,” Krumpak says. “That’s the best writing you’ve ever done.”

TJ Niebel was driving his ATV on a rural road when a deer ran into him, flipping his ATV and sending TJ into a nearby cornfield.
TJ is 36 and he’s starting over.
On Nov. 8, 2024, he was riding his ATV when he swerved to miss a deer, and a second deer rammed his four-wheeler, flipping it twice. Among his many injuries, TJ lost sight in his right eye and injured his brain. He was in a coma a couple of weeks before he opened his eyes and looked around.
Sheital Bavishi, DO, who’s managing TJ’s care, pointed to all his successes during a therapy session a few weeks after he arrived at the Ohio State Wexner Medical Center Dodd Rehabilitation Hospital.
He stood for almost an hour, with the help of therapists, and took only one short break to sit.
At times, he responded to questions correctly, picking a green “yes” card or a red “no.”
Given a washcloth, he held it up to his brow, showing he knew what the washcloth was for.
Dr. Bavishi leans her fist into TJ’s for a fist bump.
“This is the best I’ve ever seen him do,” she says.

In her role as medical director of the Traumatic Brain Injury Rehabilitation Program at Dodd, Dr. Bavishi helps people regain what they lost after an accident, stroke, heart attack or other trauma.
Some may not respond to a loved one holding their hand or saying their name, a nurse entering the room, a blaring fire engine siren. Others are minimally conscious as TJ is. He can respond to commands, but not every time.
Still, Dr. Bavishi and her team of nurses and physical, speech and occupational therapists can work with these patients. They help people relearn to walk and talk or find other ways to let their family members know what they need, what they want.
“People get better. They go back to their jobs and to their families. And those who do not recover 100%, we can teach their families how to advocate for them and care for them,” Dr. Bavishi says.
Dr. Bavishi helped launch the state’s first Disorders of Consciousness Program in 2015 for people whose traumatic brain injury left them unconscious to minimally conscious, able to make eye contact or nod “yes” or “no” to a question.
At that time, there were few other options in Ohio for treating them other than a nursing home. There, a patient’s medical needs could be met, but rarely did they get specialized therapy to help them become aware, relearn how to walk, communicate and live on their own again.

“What we’ve found is if we do early treatment, we’re able to help many people emerge,” says Dr. Bavishi, who’s also an associate clinical professor of Physical Medicine and Rehabilitation at The Ohio State University College of Medicine.
“There’s a lot we can do to give families hope.”
Dr. Bavishi’s success rate is reason to hope. Over half the patients at the Ohio State Wexner Medical Center who are treated for a brain injury that left them unresponsive or minimally responsive have regained consciousness, Dr. Bavishi says.
The night of TJ’s accident, his heart stopped before he got to a nearby hospital, his mother, Tammy Niebel, says. Medical staff restarted it.

Over two months in the hospital, TJ had 13 surgeries, many of them on his brain. Then he was brought to Dodd. Though he could open his eyes, he couldn’t track an object. He wasn’t able to turn his head to the right and struggled to hold it up.
If someone asked him to reach for an object, his left arm and left leg moved at the same time. Now he can grab something without a leg moving. He can hold his head up with less help.
“People see pictures of him and say: ‘Poor TJ.’ But where he’s at today is amazing. It’s just been one miracle after another,” Niebel says about her son.
Dr. Bavishi and her staff use a combination of medications and rehabilitation techniques to stimulate the brain out of a minimally conscious or a comatose state.
Getting out of bed and moving during the day is a key part of the rehabilitation. Physical therapists might harness the patient over a treadmill while they move the patient’s legs to encourage the return of muscle memory. Or they might place a toothbrush or a washcloth in the patient’s hand to see if the patient knows to bring it to their face.
“The biggest question everyone asks is: What’s their quality of life going to be?” Dr. Bavishi says. “There are so many unknowns. The brain heals differently for different people.”
When Dr. Bavishi first started the Disorders of Consciousness Program, she had to make a strong case to insurance companies to cover one month of intensive therapy. The thinking at the time was: How can you do rehab on patients who can’t follow commands?
But Dr. Bavishi persisted using research findings: If people with severe brain injuries receive intensive therapy within the first 90 days of their accident, they have a much better chance of significantly recovering in the long term.
“She’s developed a reputation. She’s getting people home and with services who would have never received rehabilitation otherwise.”Tracy Shannon, PsyD, a neuropsychologist for the Disorders of Consciousness Program.
As people emerge into consciousness, they may become agitated, even rebellious. That can make them difficult to work with, but it doesn’t seem to bother Dr. Bavishi, possibly because she knows it’s a sign of arousal, that their brain is recovering, Dr. Shannon says.
“Not everyone can be spit at or cussed at and stay unbiased. Dr. Bavishi does. She understands it’s an injury and not a character flaw.”

As Dr. Bavishi often reminds families: The path to recovery is a marathon — not a sprint.
At times, TJ can follow commands to hold or let go of an object, to bring a washcloth to his face, to choose between a cup or a stuffed Brutus Buckeye doll.
“He’s at the point where he’s starting to do more, but it’s not yet consistent,” Dr. Bavishi says.
That may come with time.
When TJ is released from Dodd, he’ll go home with his mom to Perrysville, Ohio, north of Columbus. She’s already bought him a dry-erase board to practice writing. She’ll buy some learning toys. TJ’s younger brother will read to him.
Before the accident, the outdoors always drew TJ, so they’ll take him outside as much as possible, and maybe he’ll remember what it was like, the thick woods, the nearby dam.
He seems to remember his dog. Whenever Niebel pulls up a photo of the feisty Pomeranian on her phone, TJ grabs the phone and won’t let go.
Niebel has seen other moments of clarity in her son as well. TJ tears up when she says goodbye. Sometimes he moves his lips like he wants to say something. Niebel hopes eventually he will.
She’s seen the progress and has been through the setbacks. She’s not having any expectations.
“I’ll deal with whatever the case may be. I put my faith in the Lord and the doctors,” Niebel says.
There’s a story Dr. Bavishi tells resident physicians. It’s about an experience she had, decades ago, when she was learning to treat people with traumatic brain injuries at Hunter Holmes McGuire VA Medical Center in Richmond, Virginia. There, one of her patients was 26 years old. He was in a coma after a car accident on a military base in Germany. All he could do was sometimes open his eyes.
After eight months of therapy and treatment, he left the hospital, walking with a walker and using a communication board to type out his thoughts.

“He came in not moving, and he left in a walker and completing full sentences,” Dr. Bavishi says.
Whenever she tells the story, the feelings she had the day he and his family left the hospital all come back. She tears up. It’s a story she tells those she works with so they understand the power of what they can do for people.
“I think it’s a chance,” she says, “to give people hope.”

Our nationally ranked team can help you recover.
Learn more