Research, experience help Blood and Marrow Transplant Program offer innovative care
Patients benefit from advances in survival rates, access, quality of life.
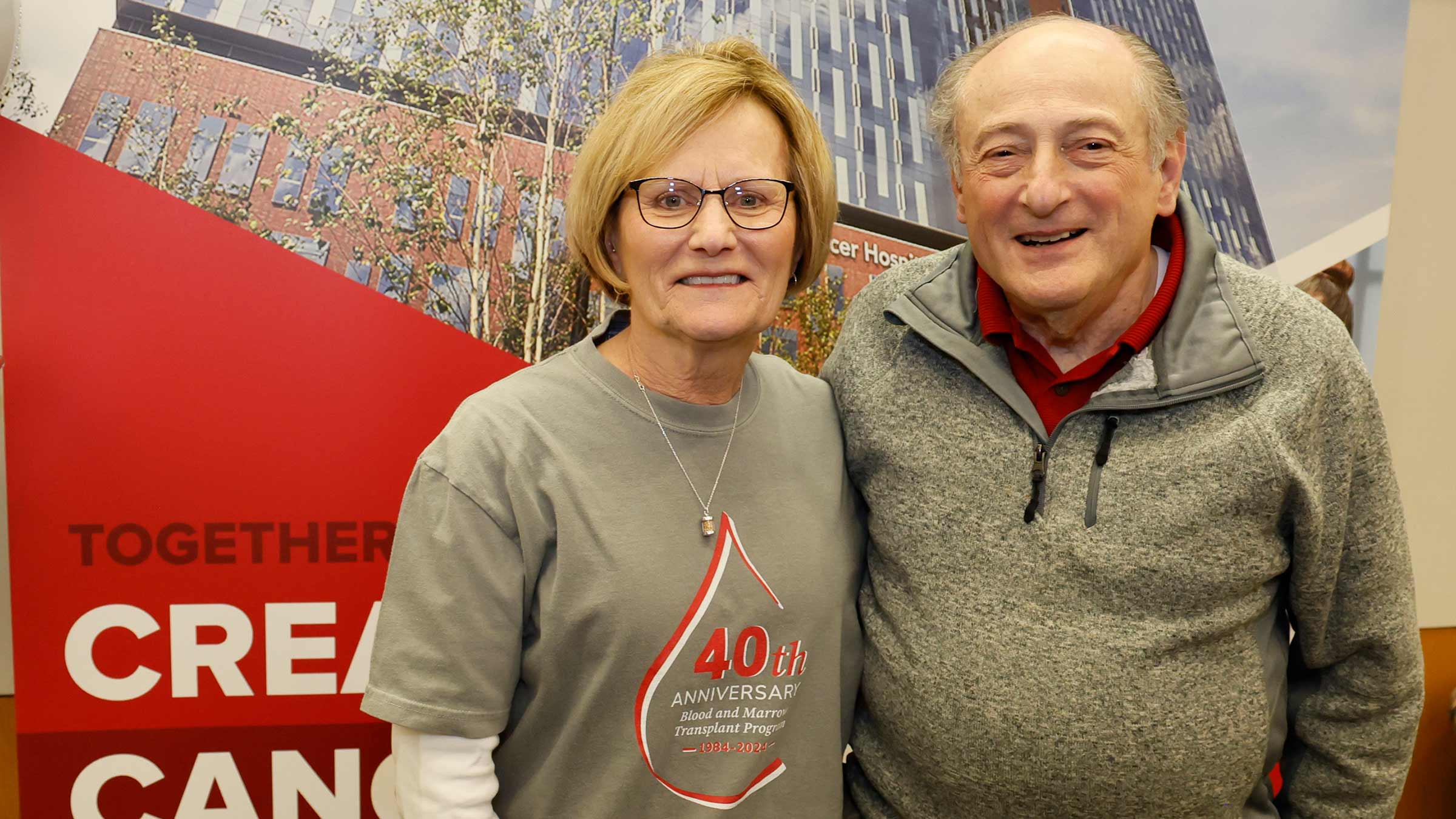
Fran Sapp and Todd Burnworth share a bit in common.
Both overcame leukemia after undergoing bone marrow transplants, and both received their transplants at The Ohio State University.
But there are some crucial differences in their stories.
For starters, Sapp was one of the first patients to receive a bone marrow transplant at Ohio State in 1984. Her hospital stay lasted six months.
Burnworth’s transplant came more than three decades later, and he was hospitalized for about six weeks.
The contrast represents just a glimpse at how far care, and science, have evolved over the past 40 years. And the newest approaches mean even fewer restrictions for today’s patients with cancer at The Ohio State University Comprehensive Cancer Center – Arthur G. James Cancer Hospital and Richard J. Solove Research Institute (OSUCCC – James).
Patients will soon start to benefit from outpatient blood and marrow transplant (BMT) and cell therapy programs at the OSUCCC – James. This means some patients could eventually receive transplants while spending most nights sleeping at home in their own beds.
A 40-year evolution in BMT care
A vast amount of knowledge and a culture of teamwork have been built throughout the BMT program over the decades, says Marcos de Lima, MD, director of the Blood and Marrow Transplant and Cellular Therapy programs at the OSUCCC – James.
“Having a program that has done 6,500 transplants and has a 40-year history, it tells you that it’s part of the DNA of the institution,” Dr. de Lima says.
Also part of the institution’s DNA is its research arm, says Marcos de Lima, MD. The team has received several private and government grants for clinical trials that bring new drugs and the most advanced treatments to BMT patients.
Such research trials not only help improve outcomes but also allow people who may not have otherwise been candidates for transplantation an opportunity to receive lifesaving care, says Sarah Wall, MD, director of clinical operations for the BMT and Cellular Therapy programs at the OSUCCC – James.
“Transplant is such a rapidly evolving field,” Dr. Wall says. “It’s still very cutting-edge, the approach. We’ve made huge leaps in progress.”
Earliest days of blood and marrow transplants
Sapp’s cancer diagnosis came after a doctor near her home in Rockford, in western Ohio, ordered blood tests for fatigue and bruising she couldn’t explain.
In her mid-30s, Sapp was not only one of the first transplant patients at Ohio State, but one of the oldest at the time. She remembers being told many of her treatments were experimental.
“I prayed that I would at least live until my boys graduated from high school,” says Sapp, who celebrated her 77th birthday in October 2024. “And here, all three of them went to college, they’re married, I’ve got eight grandchildren whom I love dearly. And I would have never been able to see them if I wouldn’t have had the transplant.”
Burnworth, of Xenia in southwest Ohio, was transplanted in 2018, in the months after pain in his right calf led to an eventual diagnosis of acute myeloid leukemia (AML).
Burnworth, who was 41, quickly became very ill, suffering complications involving his vision, breathing and kidney function. After more than a week on a ventilator, he needed occupational and physical therapy before he could return for his transplant. It seemed at that point that the complications were behind him, and “It worked almost perfectly.”
“Everyone at The James took amazing care of me. I wanted for nothing. The attention was incredible,” he says. “Overall, it was just a very smooth, well-honed, easy process.”

Advances in blood and marrow transplant care
Goals of the OSUCCC – James program have been to discover ways to prevent cancer from recurring, decrease the side effects of treatments and find more individualized approaches, Dr. de Lima says.
To make that happen, physician-scientists have helped shape sophisticated therapies that have transformed care.
Whether it’s studying ways to prevent complications, expanding access to older patients, developing first-in-human cell therapies or finding novel ways to administer cell therapies, each team member is engaged in research to offer innovative therapies and pursue higher rates of survival.
Among noteworthy achievements, the program was the only site in central Ohio to have CAR T-cell therapy before it was commercially approved. It was then one of the first programs to offer the treatment, which extracts a patient’s own white blood cells, then trains them to target and destroy the body’s cancer before reinjecting them.

“We have been witness to history, and we’ve been there from the beginning.”Sumithira Vasu, MBBS, scientific director of the Blood and Marrow Transplant Program at the OSUCCC – James.
Over the years, the toxic side effects of transplant treatments have gone down dramatically, Dr. de Lima says. In the mid-90s, about 30% of transplant patients didn’t survive one year due to problems with the transplant itself. Now, those numbers have been cut by more than half.
While the stress of transplants meant they were once reserved for the youngest and otherwise healthiest patients, advancements mean they’re now available to older people and those with more underlying health conditions, says Dr. Wall, who specializes in the effect of age on blood cancer diagnosis and treatment.

Further, the vast majority of donors now give stem cells collected from blood rather than directly from bone marrow, a much safer and less painful option with a shorter recovery time.
Donor opportunities also have expanded over the years. Historically, donors had to be matched siblings. But because experts have become better at preventing the complication of graft-versus-host disease, stem cells can now come from half-matched related donors or even mismatched, unrelated donors.
The outpatient blood and marrow transplant option
Make no mistake. Blood and marrow transplants are no walk in the park. They start with rigorous chemotherapy that wipes out the body’s immune system to make way for the transplant. Patients and their care teams must take many precautions to avoid infection as the immune system rebuilds.
This is one of the reasons hospital stays were once so lengthy and continue to be at least a few weeks for many people.
With extra precautions, the outpatient option will become available for appropriate patients depending on their cancer type and situation and as determined by their health care providers. Care teams will continue to closely monitor the status of these patients, and hospital beds will be reserved for them at the OSUCCC – James if they do need hospital care.

Sumithira Vasu, MBBS, explains that this is a critical component to ensure blood and marrow transplant patients don’t linger in emergency departments where they might be exposed to potentially dangerous infections.
“Our team knows what to expect and what can go wrong,” Dr. Vasu says. “We’ve seen it before and know what to do and how to get patients taken care of.”
Improving quality of life for BMT patients
Quality of life for transplant patients has taken a huge leap in the past four decades, Dr. Vasu says. The earliest transplant patients were tended to by doctors and nurses who wore gowns and masks akin to hazmat suits.
“Patients couldn’t shower every day or see their family members. They were extremely isolated in the hospital, going through a very intense procedure all alone, not being able to do things that give you basic dignity,” she explains.
Forty years later, adult family members can spend the night, and patients can do exercise classes together, walk the hospital halls or enjoy an outdoor patio.
“So, this is how far we’ve come from a human perspective in terms of doing these procedures,” Dr. Vasu says.

BMT gives new lease on life
During her time in the hospital, Sapp was largely separated from her three sons, who could visit only when perfectly healthy and wearing gowns and masks.
After she was released, she stayed in an apartment near the hospital for several months. She always wore a mask, everything that came in had to be sterilized and she had to forgo things like deli meat for fear of infection.
But she’s convinced she is alive today only because of the Ohio State team, and she has advice for others facing a transplant.
“Just have an open mind. Say you’re going to live, it’s going to help you 100%. It might not be the most pleasant thing. But if you don’t have it done, you’ll regret it,” Sapp says.
In more recent years, Burnworth spent his hospital time walking for fitness in the hallways, using shared exercise equipment and enjoying pancakes in a nearby hospital café.

Like Sapp, he spent the time separated from his then-11-year-old daughter, but he was thankful for the text messaging and teleconferencing that allowed them to stay somewhat connected.
When he was released, he began to gain strength by walking at the local shopping mall.
By 2024, he was hiking the Teton Range in Wyoming, making a 30-mile trek to the top of a mountain. That September, he completed an arduous 100-mile bike ride from Columbus to the Ohio River, continuing to leave cancer in the dust.
“This is all with a new lease on life. Ohio State has saved my life and given me opportunities that I wouldn’t have had otherwise,” he says. “So, I’m committed to making the most of it.”


The region’s most experienced blood and marrow transplant program
Trust your care to The James.
Learn more
Support blood and marrow transplant research
Your gift sustains advances in this work.
Donate now






