Vascular surgeon designs surgical stents that could save countless lives
Novel design holds promise to improve vascular surgery, drug delivery and expand organ donation
One evening in his family room, vascular surgeon Bryan Tillman, MD, PhD, sat shoulder-to-shoulder with his neighbor, an organ transplant surgeon named Amit Tevar, MD. Between them was a simple paper napkin. While the two talked, Dr. Tillman sketched, illustrating an idea while it was fresh in their minds.
With that sketch, Dr. Tillman expanded the possible uses for an innovative invention he was designing in his lab to replace common surgical clamps.
Doctors have used surgical clamps for decades. They stop blood flow during surgery, but they can cause complications. A patient’s legs can usually tolerate clamps easily, Dr. Tillman says. But clamps on major arteries, like the aorta, often result in complications because of the loss of blood flow.
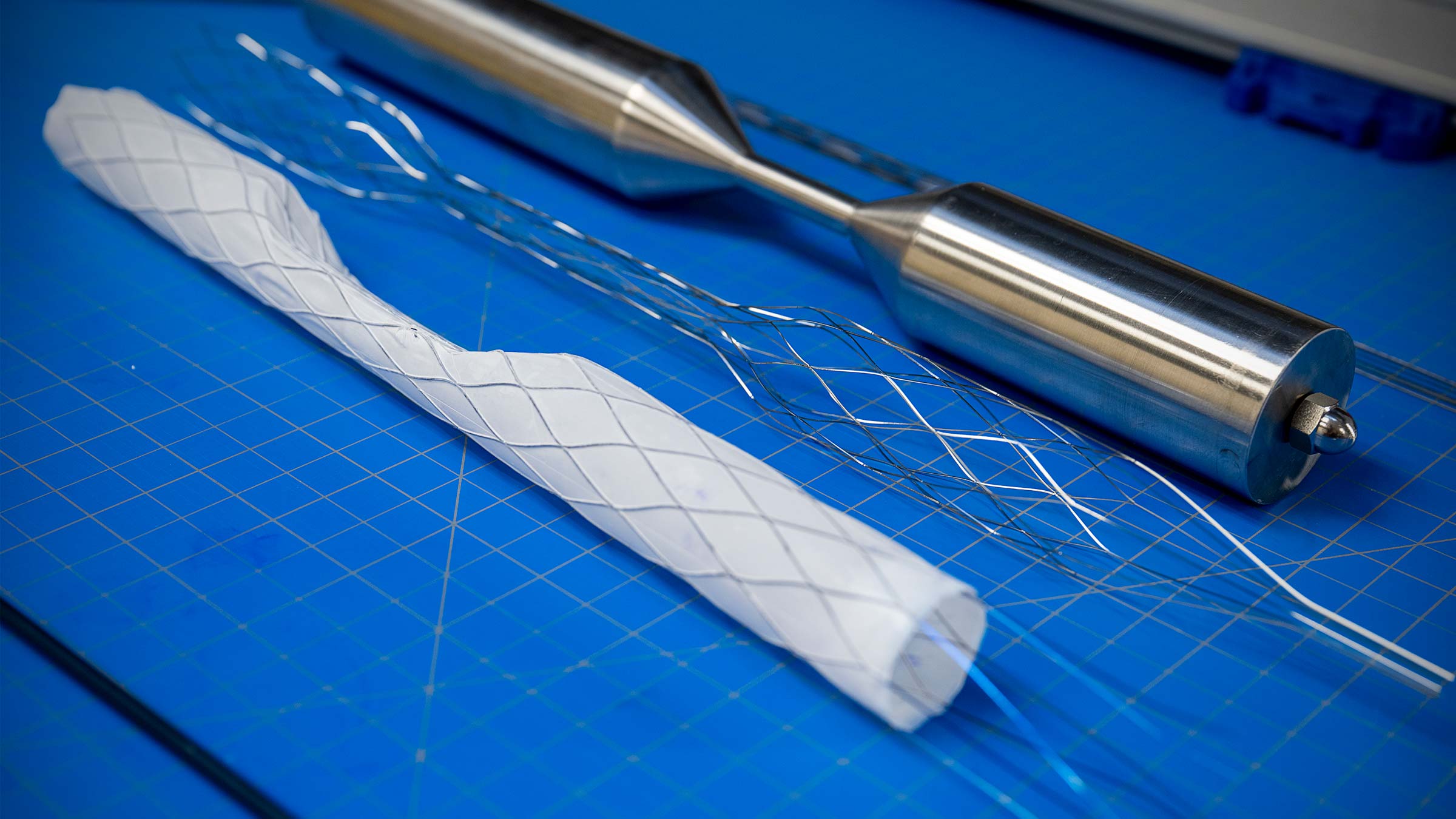
Dr. Tillman, an accomplished researcher and surgeon, had designed a retrievable rescue stent graft to overcome complications and prevent the need for clamps. His stent can be inserted minimally invasively through a catheter and deployed in the artery. This allows a surgeon to repair the vessel around the stent without actually stopping blood flow. At the end of surgery, the surgeon can remove the stent as simply as it was inserted.

With the help of his neighbor, who intimately understood the challenges of keeping organs from consenting donors viable for donation, Dr. Tillman sketched improvements to his retrievable stent so that it could be used to enhance organ donation. Later, he would realize other uses for drug delivery and even battlefield trauma. That napkin would change the course of Dr. Tillman’s research, giving his invention broader applications that could help an entirely new patient population.
How retrievable stents could change vascular surgery
Vascular surgeons treat vascular disease in most areas of the body. “The only areas we aren't involved with are the heart and the brain,” Dr. Tillman says.
As a vascular surgeon at The Ohio State University Wexner Medical Center and a professor of Surgery at The Ohio State University College of Medicine, Dr. Tillman has explained the risks of major vascular surgery to patients countless times over his 16 years in the field. To be able to eliminate complications that can come from blocking off the blood flow with clamps would make vascular procedures much less risky.
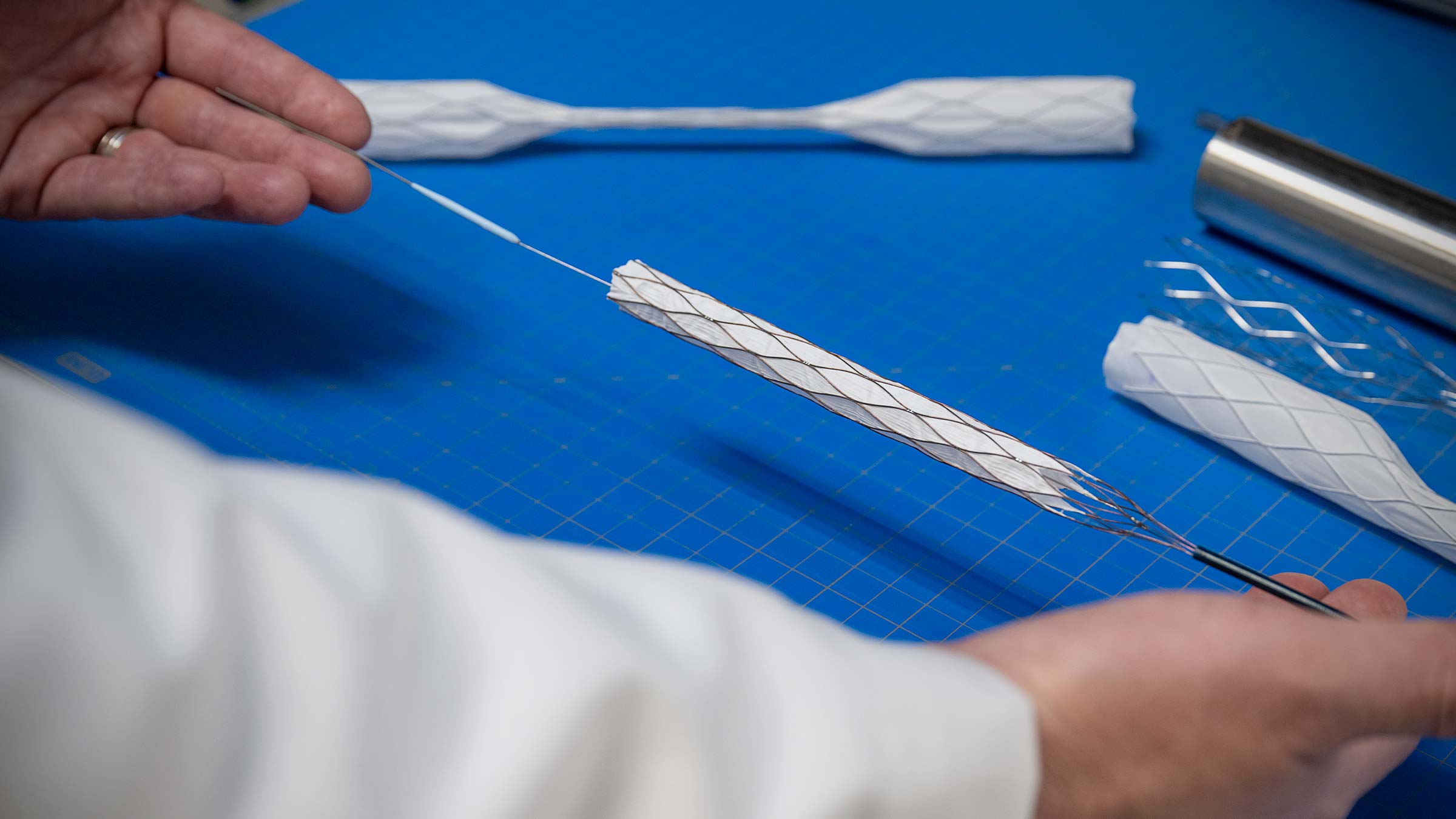
Reducing complications from vascular surgery is the main focus of Dr. Tillman’s research on retrievable stents. By changing his original design from a cylinder to a dumbbell shape, with the help of his neighbor, he’s now testing the stents in new areas, including organ donation and drug delivery.
“What really motivates me are the scientists over human history, and how one person, or small groups of people, with one idea, could really transform our world,” he says.
The retrievable stents that Dr. Tillman has been developing since 2012 are still in the research phase. He hopes he can get FDA approval within 5-10 years.
One patient sparks years of research and discovery
If approved by the FDA, the novel retrievable stent Dr. Tillman developed would be the first technology to successfully replace clamps in vascular surgery. The inspiration for the stent came from a surgery during his residency at the Ohio State Wexner Medical Center that never left his mind.
Dr. Tillman was part of a team conducting major vascular surgery when a patient’s vein was injured by a vascular clamp. It's a common injury, but it’s difficult to repair. The team tried all the usual ways to stop the bleeding, but they couldn’t see the problem amid the pooling blood. On the spot, with the clock ticking, they creatively found a way to use balloons above and below the injured vein to block the blood flow. The idea worked, the patient walked out of the hospital, and the team wrote about the case in a research paper.
That close call stayed with Dr. Tillman. There had to be a better tool for these situations. Six years later, he designed his first concept for his retrievable rescue stent while working as an associate professor of Surgery at University of Pittsburgh Medical Center. He and Youngjae Chun, PhD, an engineer in Pittsburgh, designed and constructed the first prototypes of the rescue stent.
How a simple idea became a remarkable tool for vascular surgery
Stents have been widely used as a permanent solution in vascular surgery since the early 2000s. They hold open a passage in the body, such as a weak or narrowed artery compromised from cardiovascular disease or other factors.
What makes Dr. Tillman’s idea different from permanent stents is that the device is retrievable, so it can be used temporarily during surgery.
“The retrievable stent allows you to place it rapidly in an emergency. And then, when you're done, you can just remove it,” Dr. Tillman says.
This means doctors can insert a stent under stressful conditions, without optimal imaging or vascular surgery expertise. It doesn’t have to be perfectly sized or positioned, as long as it serves the purpose of controlling bleeding during surgery or in a trauma.
Once the stent is in place, blood can flow through without spilling into the field of operation, rather than blocking it with clamps. The team can pull the stent through the sheath again to remove it from the patient’s body once surgery is complete.
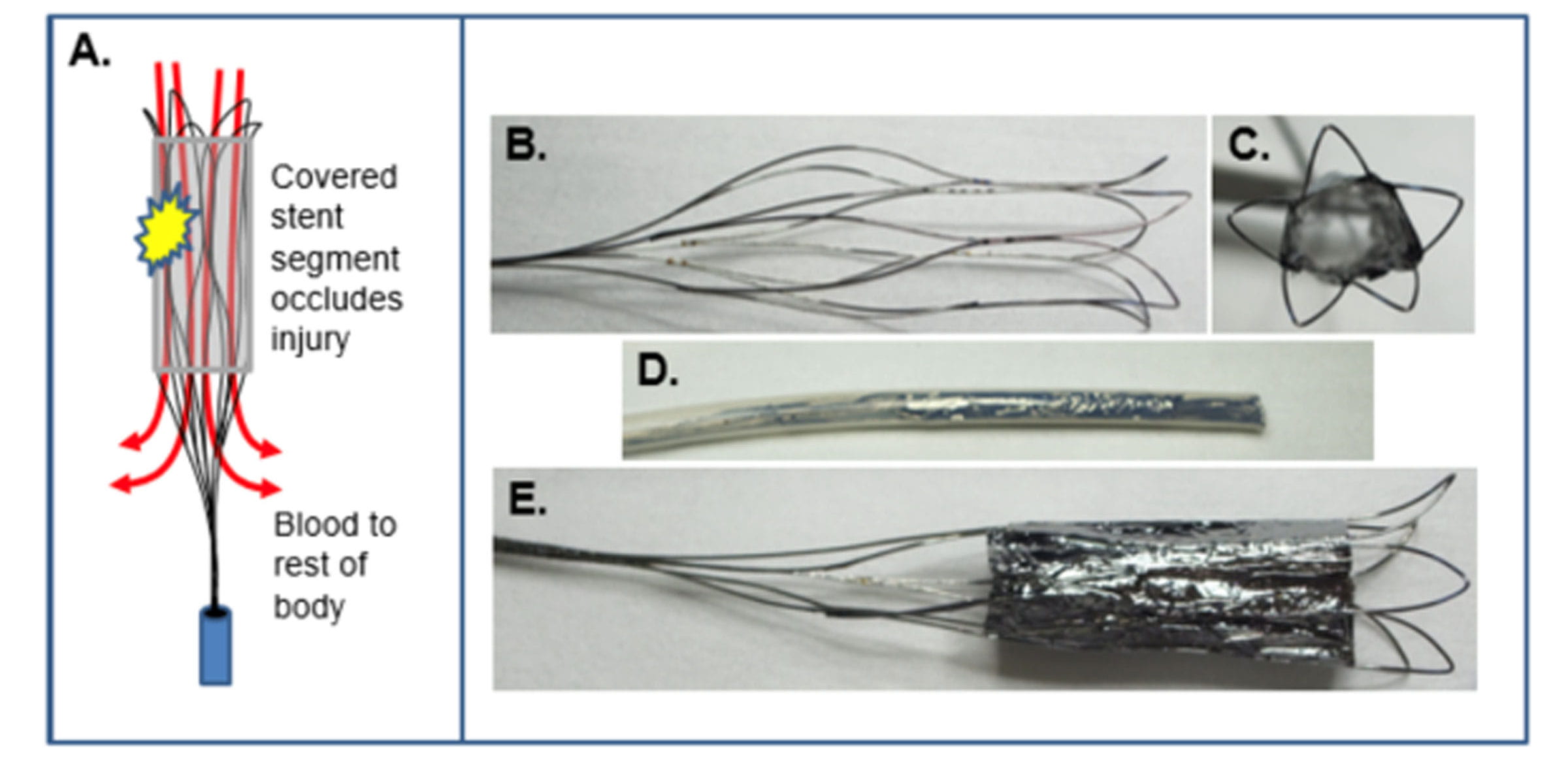
First version of the retrievable “rescue” stent graft.
“The design is simple, but its potential impact could be profound,” Dr. Tillman says.
The 2.0 version of the stent with a dual chamber, which Dr. Tillman later drew on a napkin, makes the technology applicable to even more areas of medicine.
Timur Sarac, MD, chair of vascular surgery and director of the Ohio State Aortic Center, calls the retrievable stents a “platform technology” because the device applies to so many areas of medicine.
Four uses of retrievable vascular stents
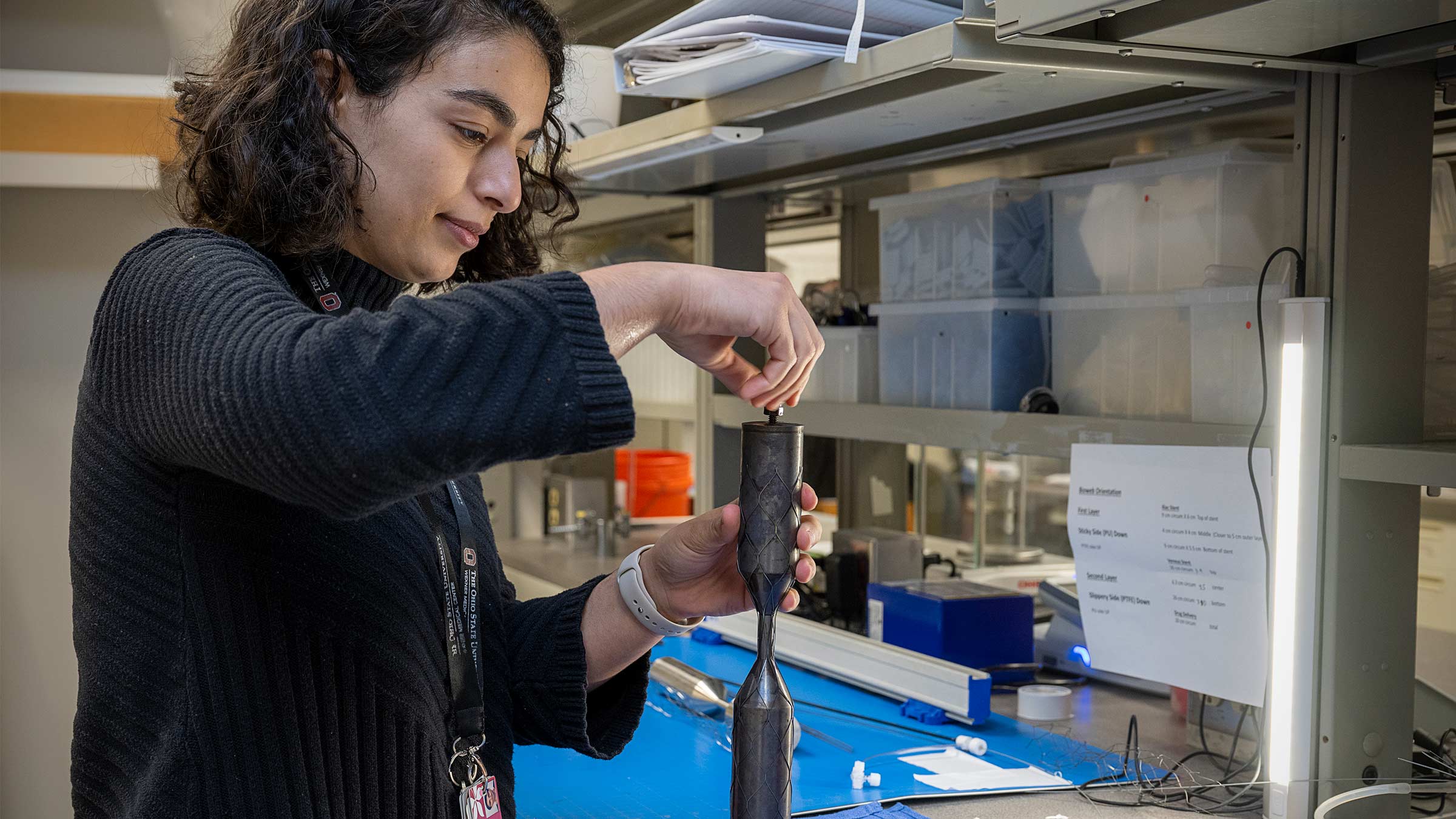
On any given day, Dr. Tillman dashes between seeing patients, managing emergencies and testing hypotheses in the lab. He’s supported by a small lab team of three, including surgical residents Dahlia Kenawy, MD, and Jordan Stafford, MD, who allow him to toggle between two significant roles. While an operating room is prepped, Dr. Tillman will meet a deadline for a federal research grant. While conducting an experiment in the lab, it’s not uncommon for him to rush out for emergency surgery.
He also mentors residents and medical students to follow in his footsteps. “He’s one of the greatest mentors I’ve ever had,” says Dr. Kenawy. “You can tell when he is teaching that he really enjoys being able to help you progress in your own career path.”
Dr. Tillman’s own career began in college when he was on a path to pursue a doctorate in medical research combined with medical school. As a child, he recalls hearing news about cystic fibrosis and wondering why some children had to shoulder this devastating burden. A young Tillman was determined to improve lives through research. During his studies, he met physicians and knew then that he wanted to be able to experience what he was investigating. “I could see patients who actually had that problem instead of just reading about them in a book,” Dr. Tillman says.
Becoming a surgeon, as well as a research scientist, wasn’t common at the time. But he wanted the ability to diagnose a problem, deliver therapy and assess patient outcomes. During his residency at Ohio State, he says, “I found surgery to be a great platform for my vision.”
Dr. Sarac recruited Dr. Tillman back to Ohio State from Pittsburgh. “He’s able to synthesize multiple pieces of information. He carries that into the research and then into the space of taking care of patients as well,” Dr. Sarac says.
Together with his lab team, there are four applications Dr. Tillman is testing for the use of the retrievable stent.
1. Approach complex vascular problems in new ways
Cutting off blood flow during surgeries is stressful for the heart and lungs and can cause organ failure and even paralysis. In spite of the risks, the technology for open major surgery largely hasn’t changed in decades.
Retrievable stents could simplify an otherwise complicated surgery. For some types of aortic disease surgery, for example, there is a high risk for complications inherent in the procedure itself. The mortality in these patients is very high, and they typically have a poor outcome. “We believe our stent graft, by replacing the vascular clamp, may reduce risks to the patient by preventing organ failure, paralysis, lung failure and heart attack,” Dr. Tillman says.
2. Treat traumatic bleeding
Dr. Tillman realized the temporary nature of his device could be a game changer for trauma care, particularly in battlefield situations. The military agreed.
With a grant from the U.S. Department of Defense, Dr. Tillman was able to test ways the stent would be useful in an austere environment where medics carry their tools on their backs. Most deaths on the battlefield are caused by loss of blood. Having a way to rapidly stop bleeding until an injured soldier can be evacuated would be a game changer.
The simple design of Dr. Tillman’s stent means that a trained vascular surgeon isn’t needed to deploy the stent. He has also developed magnetic sensors that aid in deploying and tracking the stent’s position in the body in the field, without the need for sophisticated operating room equipment.
For hospitals, the ability to deploy the retrievable stents means that residents and general surgeons can use them in the case of trauma or to triage multiple victims in situations like mass shootings.
Dr. Tillman saw firsthand how a mass shooting strains the resources of an emergency department when victims from the 2018 Pittsburgh synagogue shooting arrived at his hospital. His colleagues stood by ready to triage multiple victims who would arrive at the same time. Having retrievable stents as another tool in the trauma kit would buy more time for doctors as they treated multiple trauma patients at once.
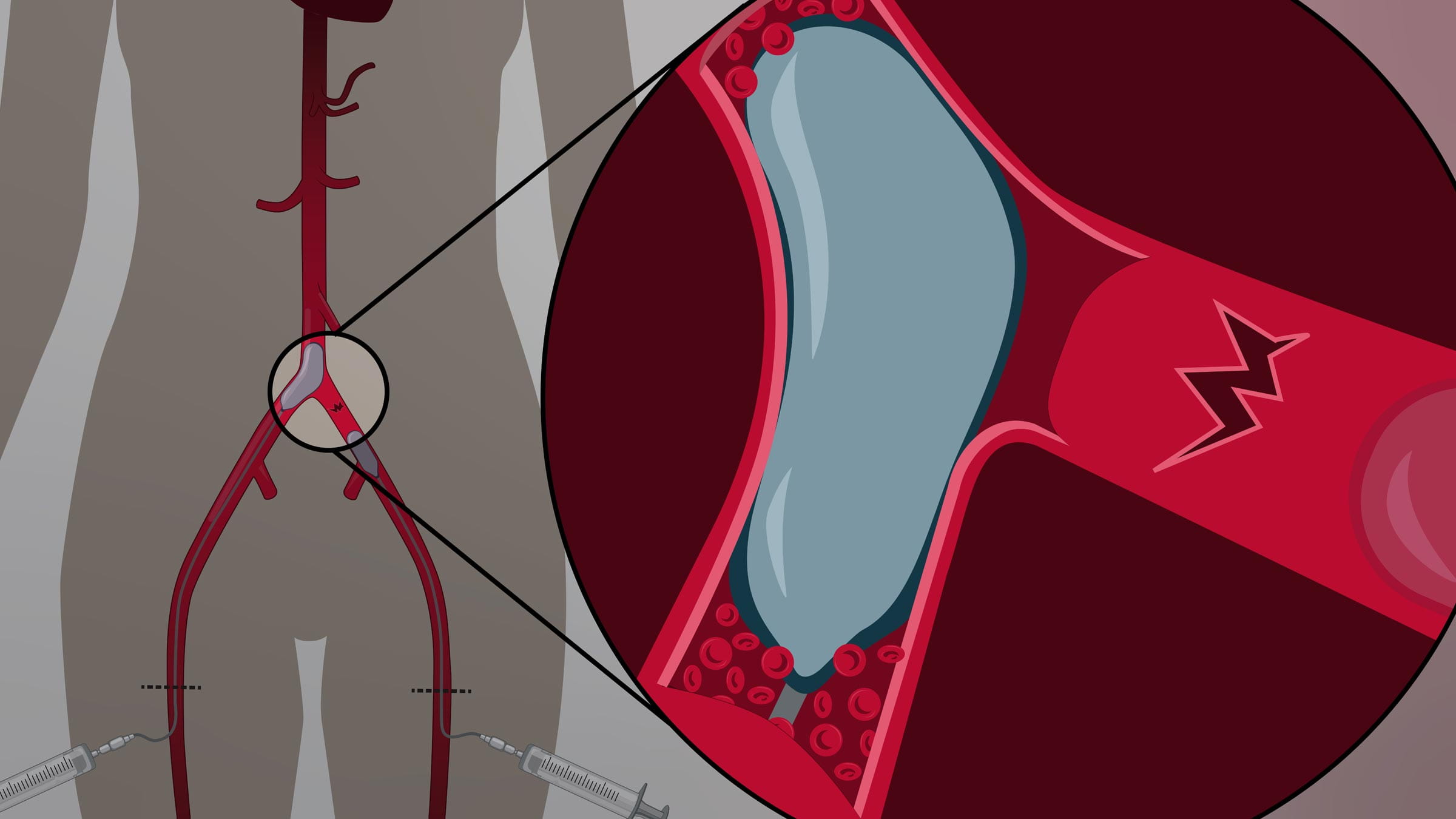
3. Improve donor organ recovery for transplantation
While there’s a critical shortage of donor organs for transplant in the United States, many organs are rendered unsuitable for donation. A method to support blood flow to organs could solve the problem.
Dr. Tillman and his neighbor back in Pittsburgh realized the novel stent could work for organ transplant, but only if it were shaped a little differently. They changed the design from a cylinder to a dumbbell shape as they drew it on the napkin. The dumbbell shape allows blood to continuously flow to organs in a minimally invasive way even while the heart is beating irregularly or not at all. “The stent allows you to put the organs on life support even while the rest of the body is dying,” Dr. Tillman says.
4. Provide focused delivery of drugs
The dual chamber design leads to other potential uses as well. Dr. Tillman realized that creating an isolated space in the vessel separate from the circulation would allow doctors to deliver potentially toxic drugs to a specific area without exposing surrounding organs and tissue.
This was a use that hit home for Dr. Tillman, whose son was diagnosed with lymphoma at age 4.

Dr. Bryan Tillman pictured with his son, Gabriel, when he was undergoing chemotherapy for lymphoma. Gabriel is now 11 and recently celebrated five years in remission.
For two and a half years, Dr. Tillman and his wife watched their son, Gabriel, undergo harsh treatment that ultimately saved his life. To be able to isolate parts of the body that need toxic drugs would make cancer treatment more manageable and less dangerous. This would allow doctors to highlight the therapeutic effect of drugs, while minimizing toxicity. “While I’m not in a position to do cancer research directly, I know what it is like to feel hopeless,” he says. “I hope that someday soon, the work that we do may positively impact others.”
Dr. Tillman and his team are also exploring a way to use these stents to make a window into the spinal cord to directly infuse drugs. Instead of inserting needles into the spinal cord, they can send the drugs through a stent in a blood vessel, which is less invasive.
Throughout his career, Dr. Tillman has maintained a steadfast commitment to improving patients’ lives through vascular surgery. He’s always thinking about how to solve problems, get a better outcome or do something more easily.
“If you’re a good surgeon and you save a patient’s life, that impacts one patient. If you fundamentally change how we approach a clinical problem, you could save thousands or even millions of patients.”

Your heart is in the right place
Learn more about advances in care and treatment for patients at The Ohio State University Heart and Vascular Center.
Expert care starts here