People want hip or knee replacements in order to return to an active lifestyle.
While it’s statistically uncommon to get a joint infection after a joint replacement, these infections do represent the most significant complication associated with a new prosthetic joint. And a serious bacterial infection can be hard to combat.
The complexities of periprosthetic joint infections
Antibiotics often don’t work near prosthetic hardware, for multiple reasons. Hip and knee replacements can create an ideal environment for bacteria to thrive.
An infection can mean more surgeries to flush out the infection, possibly a revision of the replacement and could leave someone immobilized.
That’s why there’s so much research and effort that go into keeping people infection-free before they even enter an operating room for their joint replacement.
How joints get infected
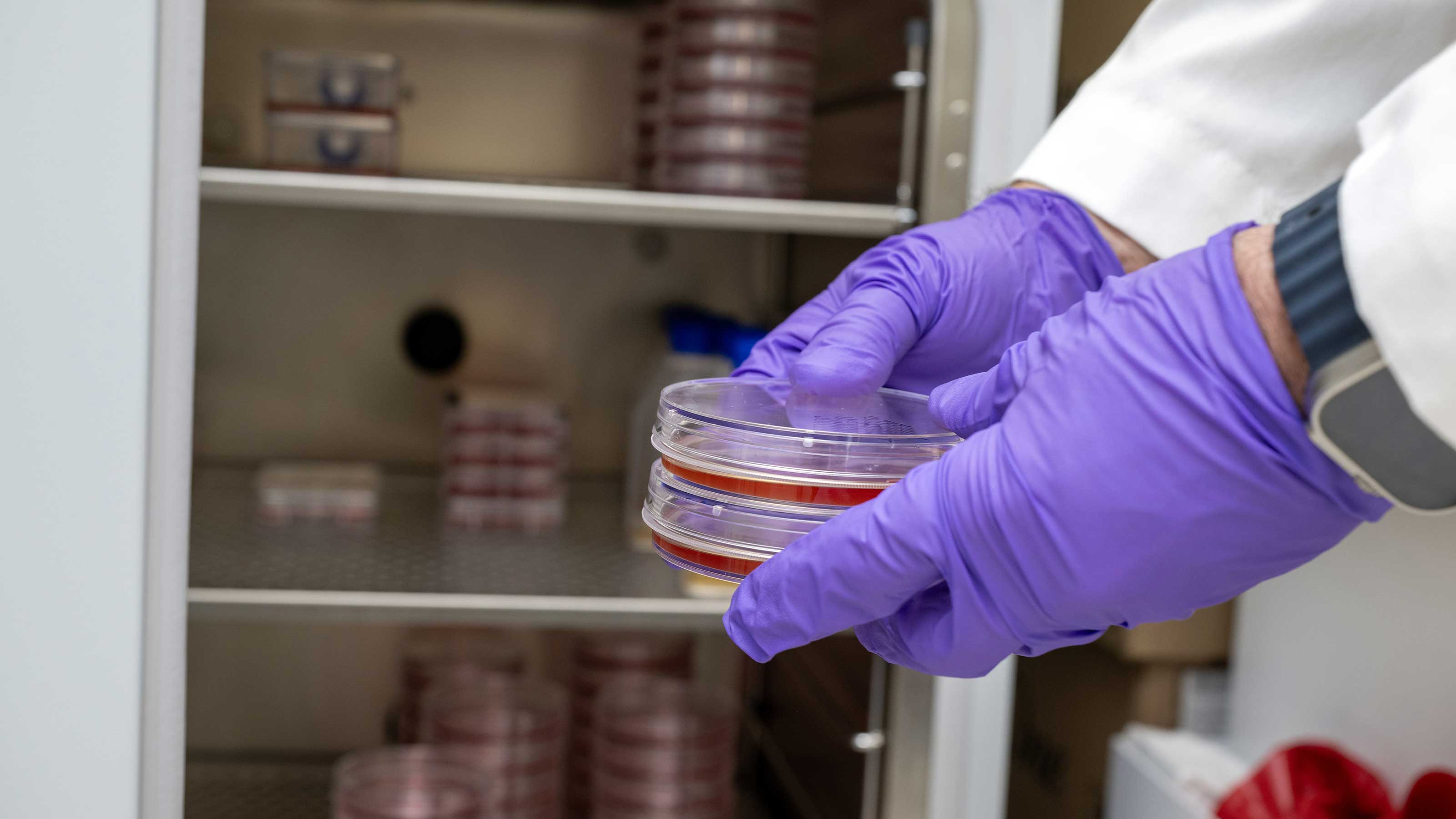
A slimy substance called biofilm can develop in as little as 10 minutes. The material is a complex polysaccharide matrix created by bacteria for protection. And antibiotics often can’t get through that protective barrier.
Fomites – particles like your dead skin cells or dust – can travel by floating through the air. In the operating room, bacteria can sometimes get carried on those little floating fomites, and they can land in a surgical area and then cause an infection.
Periprosthetic joint infections can begin after exposure during surgery or even from unrelated infections years later.
A chest abscess, severe bug bites, infected cuts or even dental infections can cause bacteria to enter the bloodstream, often making the prosthetic joint area a prime spot for infection to develop.
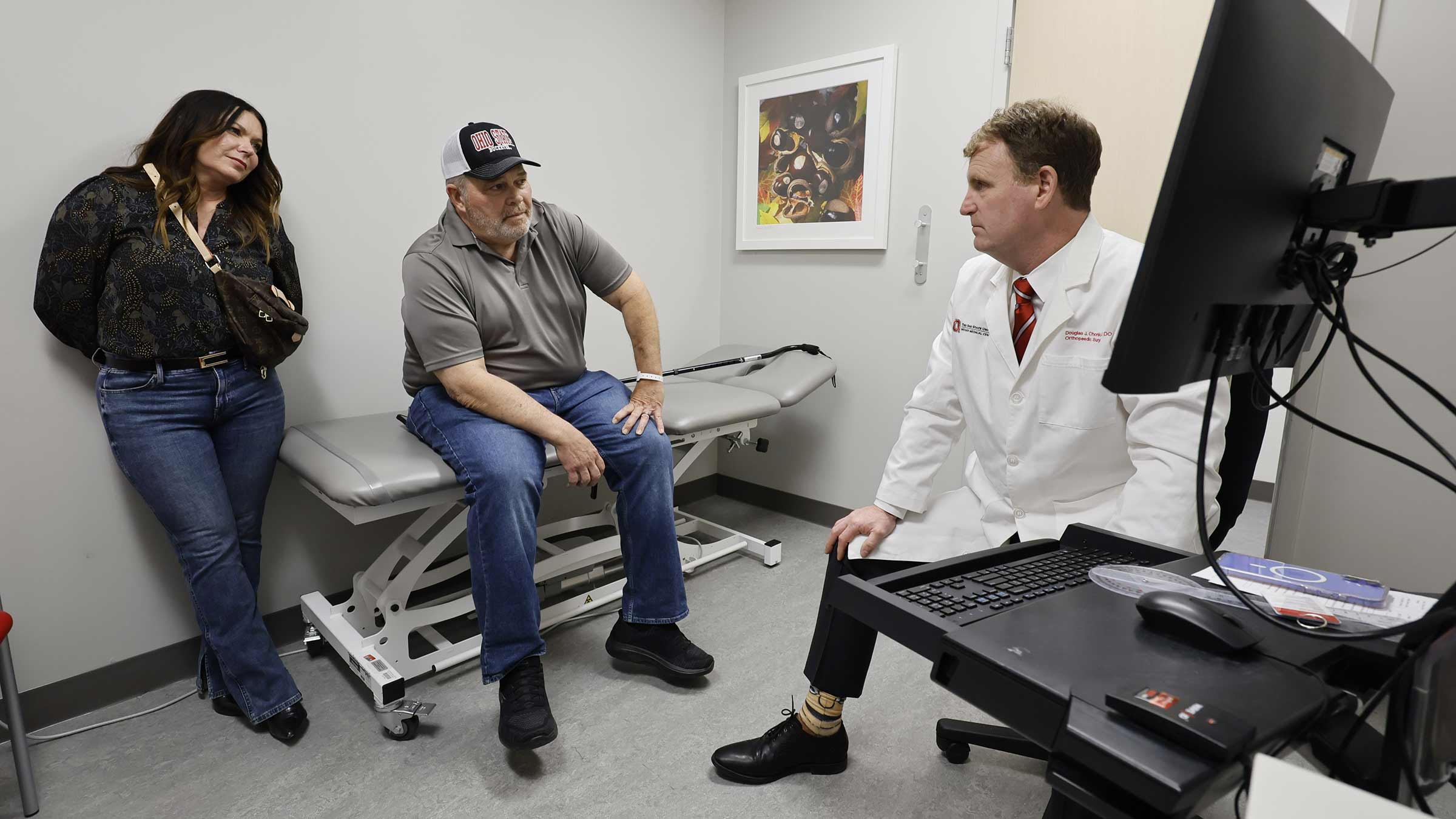
Why it can be hard to diagnose joint infections
Diagnosing infections can be difficult when there isn’t an apparent festering wound or incision.
There is no single blood test to diagnose a joint infection. Sometimes infections can be visible on scans but not always.
Here are some signs someone could have a joint infection:
- Patients may report not feeling as well as they used to. Feelings of fatigue and low energy are common.
- Cold-like symptoms may be present.
- Pain and limited mobility can occur.
Getting you ready for a joint replacement
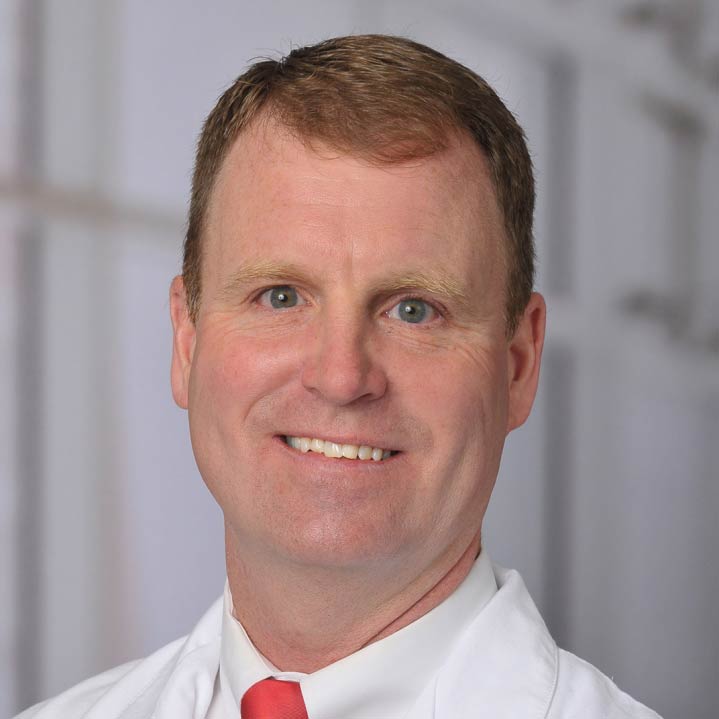
Doctors look at whether each person has health issues that could complicate surgical outcomes for replacements.
Any underlying health conditions that might raise infection risk have to be addressed before surgery. Some examples include:
- Diabetics should have an A1C below 7.
- Those who are overweight need to have a BMI below 40.
- Anyone on drugs that suppress the immune system must be able to take a break for a month or two to have the surgery.
- Anyone who smokes needs to quit.
- No steroid or other injections can be used in the affected joint for at least 3 months prior to surgery.
We don’t recommend joint replacement for patients that are on renal dialysis, have end stage liver failure, are currently undergoing chemotherapy or take medications that compromise their immune system, if they’re unable to stop those medications.
Lowering the risk of joint infections
We’re always researching and doing everything possible to stave off infections. Once someone is cleared for surgery, we partner with them to lower the risk.
- Take a breath and inhale: Nasal sprays that kill bacteria are administered ahead of surgery. This measure has been shown to decrease risks and reduce infections by up to 50%.
- Antibiotics on target: Surgeons inject antibiotics, intraosseous infusions, directly into the bone – right where they're needed most. IV antibiotics within an hour of surgery are given to all patients.
- Prep, clean and repeat: Chlorhexidine scrubs are sent home to clean the area ahead of surgery.
- Suit up: Surgeons wear surgical helmet systems resembling space suits, equipped with fans and air filters to protect patients from potential infections.
- Take your medicine: IV antibiotics are prescribed and taken ahead of the surgery.
- Checkups matter: Dental clearance must be obtained before surgery, and antibiotics must be taken before each dental visit for one year to lower infection risks.
- Targeted defense: For knee replacements, we keep the tourniquet up during the infusion to localize the antibiotic effect.
How we’re trying to change outcomes
Bacteria always evolve and find ways to survive, and, while most areas of medicine have advanced, outcomes in orthopedic infections haven’t improved, and they might have worsened over the past 25 years because of the ongoing emergence of resistant bacteria.
Researchers are looking at other alternatives, such as bacteriophages, which are viruses that eat bacteria.
Ohio State is part of a multi-center study evaluating spacers that irrigate the knee and hip joint with antibiotics that can fight infections in a short amount of time (7-10 days).

Challenging bacterial joint infections are life-altering
Ohio State’s Musculoskeletal Infection and Periprosthetic Joint Infection Program is committed to fighting infections.
Learn more