Neurosurgeon’s breakthrough in gene therapy offers new hope for brain disorders
Therapy pioneered by Russell Lonser, MD, could usher in new era in treating Alzheimer’s disease and other brain disorders.
Infusing medication directly into the brain stem of an infant was viewed as risky by many, but neurosurgeon Russell Lonser, MD, knew it might be the boy’s only chance for survival.
The child’s parents agreed, and the surgical team went ahead with the experimental procedure.
While it was a success, the boy later died from other complications of his genetic condition, type 2 Gaucher disease, often affecting the spleen and nervous system, with a life expectancy averaging less than two years.
Still, the bravery of his parents provided a spark that has kept a decades-long fire blazing within Dr. Lonser, who has spearheaded innovations that helped spur some of the biggest gene therapy advances in a generation.
“At the time, people thought we were crazy to infuse in the brain stem, that this child would die,” Dr. Lonser says of the 2004 procedure. “It was terrifying. No one had ever done it before. But if it had not been done, similar surgical breakthroughs would not have happened.”
Through groundbreaking innovations in brain therapy delivery, Dr. Lonser has helped propel The Ohio State University Wexner Medical Center to the forefront of neurological disease gene therapy treatment, turning pioneering procedures into promising new hope for patients worldwide.
“There will always be risk. There’s no other way to make progress,” he says.
Neurosurgery research could transform millions of lives
Twenty years after that initial critical surgery, Dr. Lonser was overseeing an experimental surgery, again involving a young child. This time, the procedure was being used to deliver a gene therapy, with the help of an advancement he pioneered that allows surgeons to precisely monitor the therapy’s movement as it’s infused into the brain.
Paired with the discovery of another researcher who has now joined him at Ohio State, it’s a once-in-a-generation breakthrough that could represent the holy grail for today’s neurological field, potentially giving surgeons the ability to cure conditions like Alzheimer’s disease and Parkinson’s disease by delivering growth-factor genes to rescue dying brain cells.
“If it has the ability to reverse disease, that changes the lives of millions of people in the United States overnight. It would completely reshape how we think about disease,” Dr. Lonser says.
Clinical trials at the Ohio State Wexner Medical Center and The Ohio State University Comprehensive Cancer Center – Arthur G. James Cancer Hospital and Richard J. Solove Research Institute (OSUCCC – James) have achieved initial success with Huntington’s disease and with a rare childhood disorder called AADC deficiency, and they’re poised to bring treatments to countless patients within the next decade.
About a dozen trials are in progress for a range of conditions including Parkinson’s disease and Alzheimer’s disease – with both environmental and genetic causes – for people who are in early to moderate stages of disease.

Gene therapy breakthroughs built on decades of research
The 2004 brain stem infusion in which Dr. Lonser participated was done at the National Institutes of Health (NIH) using an innovative method devised by his mentor, the late Edward Oldfield, MD.
Dr. Oldfield is recognized as a pioneer and as one of the most impactful neurosurgeons historically, says Dr. Lonser, who completed a research fellowship at NIH before joining the staff there and subsequently becoming director of the Surgical Neurology Branch, a position he held for five years before moving to Ohio State in 2012.
“A lot of what I learned from him I still carry with me in my career. It’s having the conviction to finish the things you are doing for a larger goal; it’s being unwavering when you need to be unwavering,” Dr. Lonser says. “He was absolutely driven in changing neurosurgery. He didn’t dabble in anything.”
Early clinical trials in delivering immunotoxins to cancerous glioblastoma brain tumors extended survival, but larger trials were failing because surgeons were delivering medications that weren’t making it to their targets.

“While people were doing this for 20 years, no one had any idea where the drug was going. It was done blindly,” Dr. Lonser explains. “So, trial after trial failed, even though the early data was quite positive.”
By the early 2000s, Dr. Lonser and Dr. Oldfield had developed the process that allows surgeons to monitor the infusions in real time. Then, in 2008, Krystof Bankiewicz, MD, PhD, who had also worked at NIH and was working at the University of California, San Fransico, at the time, developed a system for delivering deactivated viruses that transport genes into the brain. This system allows surgeons to place these gene carriers into brain circuits, sending them in any direction, or keeping them in a single location, depending on the condition being treated.
By combining Dr. Lonser’s monitoring system with Dr. Bankiewicz’s delivery system, surgeons were for the first time able to treat entire brain circuits from a single infusion.
“That was a huge breakthrough. Not in any stretch of imagination did we think we could change complete massive circuits within the brain,” Dr. Lonser says.
Dr. Bankiewicz, the Gilbert and Kathryn Mitchell Chair, joined Dr. Lonser at Ohio State in 2019, and together with Arthur Burghes, PhD, a professor of Biological Chemistry and Pharmacology, they now lead The Ohio State University Gene Therapy Institute.
A safer, more targeted gene therapy
During the clinical trials that are now underway at Ohio State, surgeons drill a hole in the skull and position a cannula – a tube that is placed within a submillimeter of accuracy – into the brain. (A submillimeter is about the width of a human hair.)
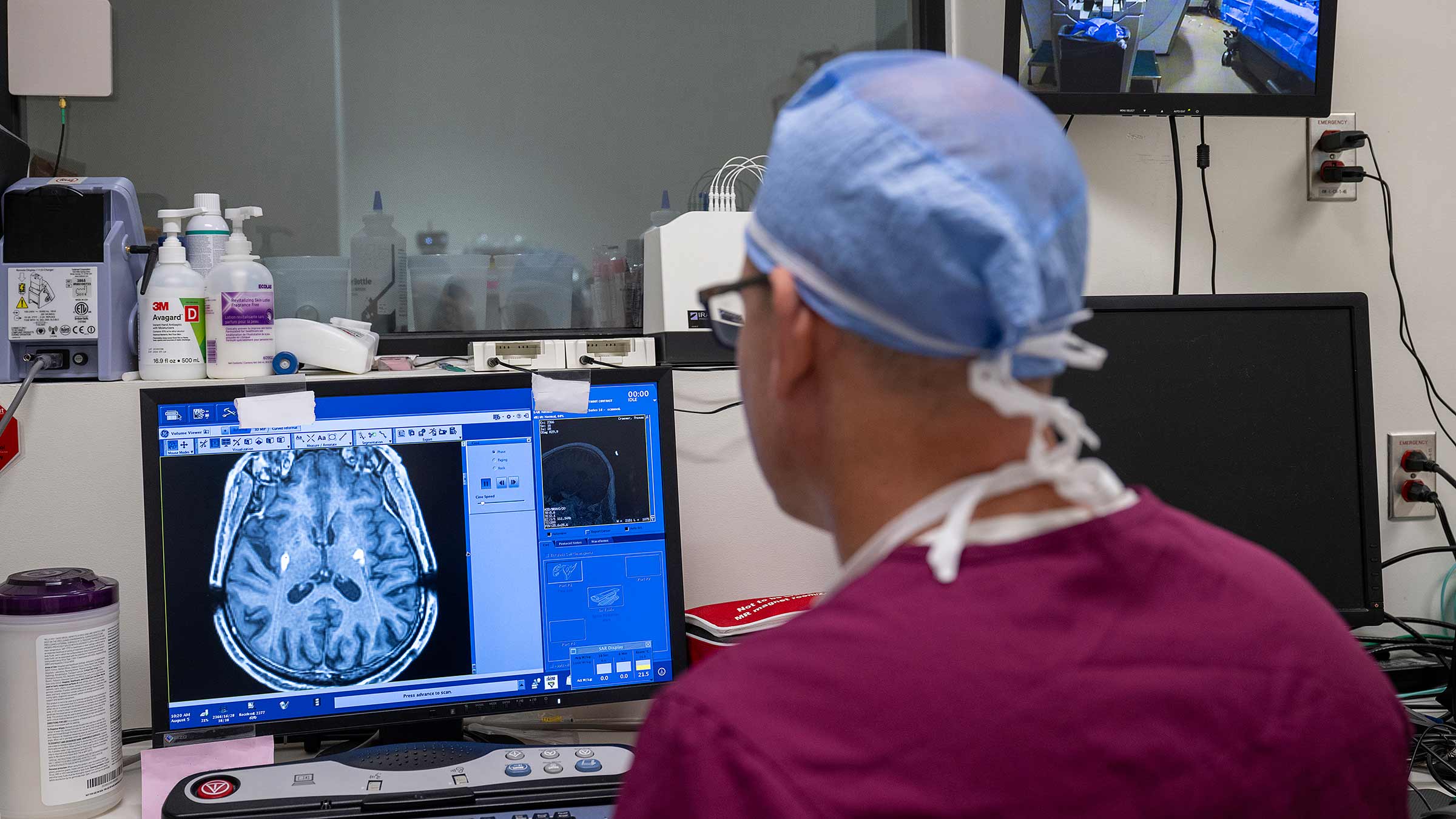
Over several hours, a powerful infusion is injected into different diseased areas of the brain as the patient continuously undergoes MRI scans.
The infusions, once they are pushed through the cannulas, provide targeted genetic treatment.
Potentially life-changing therapeutics are delivered precisely to targeted structures within the brain to treat damaged areas or cells, says Brad Elder, MD, a professor of Neurological Surgery, who performs the gene therapy surgeries with Dr. Lonser’s team. The infusions are only made once but sometimes are required in two to six areas in the brain.
“There are different strategies,” Dr. Elder explains. Therapeutics can replicate disease-free genes. When correcting a disease, genes can code for enzymes to change the way neurotransmitters behave. They also can code for a molecule to help improve neuron health.
Thanks to Dr. Lonser’s advances, real-time scans help surgeons monitor the infusion’s path, ensuring effective and safe treatment.
“We can see the infusion expand and expand. It’s important because we know how much we’re treating. We know when we can stop,” Dr. Lonser says. “It adds a level of safety to it because we’re not going to infuse outside that structure.”

The technology has already successfully treated the rare AADC deficiency, allowing children who previously couldn’t talk or walk to reach milestones once thought impossible.
Recently, trial results in partnership with a gene therapy company, UniQure, showed a majority of people with Huntington’s disease experienced a slowing progression of the disease during a 35-month trial. Ohio State performed most of the surgeries in the United States.
Dr. Elder credits Dr. Lonser with making Ohio State a national leader in gene therapy for neurodegenerative disorders, and calls him a leader in developing the techniques that have allowed the field to blossom.
“There are some people who have a real, natural talent for getting to the bottom of a scientific question, thinking, ‘How are we going to get from here to there and how are we going to get there quickly and effectively?’ And he’s just got a real talent for knowing which pathway to pick to get there,” Dr. Elder says.

Applying new gene therapy methods to other diseases
Much of Dr. Lonser’s early work centered around treating tumors or surgically removing them from the brain and spinal cord. Today, he still spends time in the operating room removing complicated tumors from patients.
“I always love operating. It will always be that way,” he says.
It was Dr. Lonser’s original pursuit of new therapies for malignant glioblastomas that inspired the research that led to the real-time monitoring innovation.
Dr. Lonser has plans to renew clinical trials to explore targeting these brain tumors with his new methods.
It’s just one of the potential applications of the procedure beyond gene therapies.
Along with delivering immunotoxins to brain tumors, Dr. Lonser says it’s been used experimentally to deliver chemotherapy drugs and antibodies. The process could be used to treat stroke, epilepsy, substance use disorder and other conditions that affect the brain.
“It could be anything,” Dr. Lonser says.
The procedure remains experimental, and its various uses will require approval by the U.S. Food and Drug Administration.
Continuing the push for gene therapy innovation
Dr. Lonser’s work has drawn interest from industry partners seeking to develop treatments and has allowed for the development of a robust research arm that will usher in the next wave of breakthroughs, Dr. Elder says.
Dr. Lonser not only has a scientific mind but also has built a strong team and secured the right partners and needed grant funding – all of which have allowed him to make significant progress in patient care and push research forward, Dr. Elder says.
The surgeons have also started training others around the world on gene therapy techniques, including those in the United Kingdom, Poland and France, as well as Scandinavian countries.
“There are millions and millions of people who stand to benefit, and Ohio State is far and away leading in this field,” Dr. Elder says. “There are lots of reasons for that, and they all point back to Dr. Lonser.”

Ohio State’s Neurological Institute
Pioneering discovery and expert care for neurological disorders.
Learn more



